The effect of crowding on access and quality in an academic ED
Original Contribution
The effect of crowding on access and quality in an academic EDB
Teri L. Vieth MDa,*,1, Karin V. Rhodes MDb,1
aDepartment of Medicine, The University of Chicago, Chicago, IL 60637, USA
bDepartment of Emergency Medicine, University of Pennsylvania Hospital, Philadelphia, PA 19104, USA
Received 27 February 2006; revised 27 March 2006; accepted 28 March 2006
Abstract
Background: Emergency department crowding has the potential to cause undesirable outcomes. We evaluated ED access and provider and patient assessments of quality.
Methods: This multimethod study, done in an Urban academic ED, included descriptive analysis of administrative records, paired physician and nurse provider surveys, and pre- or postpatient surveys regarding expectations and experiences. Our outcomes were rates and characteristics of patients who Left without being seen , provider ratings of crowding/compromised care, and patient satisfaction. Results: During data collection periods, 11743 patients registered, and 9% LWBS. Patients who LWBS tended to be younger than 45 years (relative risk [RR] = 1.7; 95% confidence interval [CI], 1.5-1.9), of nonurgent/stable triage acuity (RR = 3.1; 95% CI, 2.5-3.8), and without insurance (RR = 1.5; 95% CI, 1.3-1.7). Seventy-four percent of all patients had insurance, and 28% were private. Doctors and nurses had 81% agreement (j = 0.54) in their assessment of crowded conditions, which were temporally associated with LWBS rates ( P b .01). In 47% of 57 shifts, at least 1 provider felt that crowding was compromising quality of care. Of 423 sequential ED waiting room patients approached, 310 (73%) enrolled and 174 (56%) of these completed phone follow-up. On average, patients felt that they should be seen within 1 hour but expected to wait for 2.1 hours. Patient’s perceived that wait times on follow-up averaged 3.5 hours, 5+ hours for LWBS patients. Visit satisfaction was inversely related to patient’s perceivED wait times.
Conclusions: We find that ED crowding increased LWBS rates and patient satisfaction. Systemwide changes in ED organization will be necessary for the ED to fulfill its role as a safety net provider and meet public health needs during disaster surge capacity.
D 2006
B This project was funded in part by a grant from the Henry J. Kaiser Family Foundation. Karin Rhodes, MD, is supported by NIMH no. K23/PA-00-004.
* Corresponding author. Tel.: +1 773 363 7768; fax: +1 773 363 7768. Reprint requests: Karin V. Rhodes, MD, Department of Emergency Medicine, University of Pennsylvania Hospital, 3000 Spruce St, Ground Ravdin, Philadelphia, PA 19014, USA.
E-mail addresses: [email protected] (T.L. Vieth)8 [email protected] (K.V. Rhodes).
1 Both authors contributed equally to the study and the manuscript.
0735-6757/$ - see front matter D 2006 doi:10.1016/j.ajem.2006.03.026
Introduction
Currently, many emergency departments (EDs) are underfunded and overcrowded [1,2]. The reasons are multifactorial. According to the Centers for Disease Control and Prevention report, between 1993 and 2003 the number of EDs decreased by 12.3%, whereas the number of ED visits increased 26%, that is, 113.9 million per year [3]. This increase in ED visits has been attributed to population growth, less access to primary care, and greater numbers of Uninsured patients [4]. During the same period, many hospitals have downsized and decreased the number of available inpatient beds. This has resulted in ED bboardingQ of already admitted patients. Additional strains to ED resources are thought to include managed care restrictions and expanding paperwork requirements [5,6].
Emergency department crowding is a reflection of financially constrained hospitals. Many blame the Emergen- cy Medical Treatment and Active Labor Act (EMTALA), which requires hospitals to provide medical screening and emergency treatment to all patients regardless of ability to pay [1,7]. However, this unfunded federal mandate for emergency care is not a new obligation. EMTALA legislation was enacted in 1986, and EDs have always been expected to provide bCharity care,Q an expectation formal- ized in 1946 by the Hill-Burton Act [8]. With decreased Medicare and Medicaid funding and lack of reimbursement for Uncompensated care, the EMTALA obligation became a significant liability [1,6]. Long wait times and crowded conditions have become common, particularly in urban EDs [9,10]. The 2000 National Hospital Ambulatory Medical Care Survey found that average ED Waiting times for nonurgent patients increased 33% over the prior 3 years [11]. This situation has the potential for undesirable medical outcomes, such as decreased staff productivity, miscommu- nication, and Medical errors, as well as extended pain and suffering and patient dissatisfaction [7].
Our research goals were to assess the effect of ED crowding on patient access and quality of care in our urban academic ED. We hypothesized that as wait times rose, 2 groups would be most likely to leave without being seen (LWBS): the nonurgent patients because they were less sick and the privately insured because of greater access to other healthcare options. We also hypothesized that ED provider ratings of crowding would be temporally associated with rates of LWBS patients. Finally, we anticipated that if expected wait times exceeded what patients deemed accept- able, their perception of care quality would be affected.
Methods
Study design
We undertook a multimethod approach to our assessment of access and quality. We measured patient access, or lack thereof, by rates of ED patients who were triaged and
registered for care, but left before called for treatment (referred to as LWBS). To identify the timing and character- istics of patients who LWBS compared with those who remained, we used ED administrative records to gather information on patient demographics, insurance status, and triage severity. These data were sampled from all seasons of the year, excluding holidays. To assess the effect of crowding on quality of care, we sought the opinions of ED attending physicians and charge nurses in real time. Their opinions were correlated with the rates of patients who LWBS. Finally, the expectations of ED patients were assessed prospectively by surveying patients in the waiting room and by a follow-up phone call to assess their satisfaction with care approximately 1 week after their ED visit. Consent was verbal for all medical staff participants who were also given written information on the study and the option to decline or withdraw from participation. Patients enrolled in the study during their ED visit via an initial written survey and HIPAA (Health Insurance Porta- bility and Accountability Act of 1996) release. The hospital’s international review board approved the study.
Setting
The site for this study was the adult ED within an urban university hospital, which sees approximately 48 000 patient-visits per year. The patient population is 91% black, 7% white, and 1% Asian. As with many Urban academic medical centers, our institution is currently experiencing high rates of crowding, with LWBS rates as high as 11% [12]. Although this rate may be consistent with comparable institutions, it is much higher than the nationwide average of 1.7% and recommended rate of 1% [3,13,14]. Upon arrival, all patients are triaged and registered, with visit-related variables manually entered into a paper ED registration log. At triage, patients are classified into 1 of 5 institution- defined acuity categories. Patients classified as red are emergent (imminent life- or limb-threatening conditions), requiring immediate treatment. For nonemergent patients with a condition that requires medical treatment, they are assigned to 2 levels of urgent categories. Patients with a potentially unstable condition are placed in the yellow category and must be reassessed if not seen within 2 hours. The remaining urgent patients are classified in the stable urgent or orange category, which does not require reassess- ment unless an unexpected deterioration in the waiting room occurs. All other patients are deemed nonurgent and categorized as green (nonurgent) or blue (very minor nonurgent cases such as wound checks or suture removals).
Administrative data
To identify the characteristics of patients most affected by ED crowding, we used data from the ED registration log and compared demographic features of patients who LWBS with those who waited for care. The ED patient registration log is a written document that documents time of arrival and
departure, insurance status, triage acuity, means of arrival, disposition (discharged, admitted, transferred, LWBS, or left against medical advice), and basic demographic in- formation for all patients. Consecutive patient data were gathered from 4 sample periods in 2003 for a total of 13 weeks of data. The first sample period was selected to overlap with the provider survey time frame (winter). The remaining sample periods were deliberately chosen for the spring, summer, and fall to exclude seasonal variation in the results. The final 2 data collections were also matched to patient survey collection periods.
Provider survey
From the providers, we collected serial ratings of ED crowding and perceived effect on patient care. The provider survey and the first administrative data sample were initially collected during a multisite effort to define measures of ED crowding and their relation to hospital inpatient capacity [15]. During each shift, at 6-hour intervals, the attending physician and charge nurse simultaneously rated the level of crowding from not busy (1) to extremely crowded (5) on a 5-point Likert scale. If the provider considered the ED crowded, they indicated the level to which crowding was compromising quality of patient care, from strongly disagree (1) to strongly agree (5) on a 5-point Likert scale.
We wanted a site-specific assessment of providers’ ability to know crowding when bthey see itQ even though scientific measures may be difficult to define [5]. To do this, we corre- lated the average ED crowding rating of the 2 providers with rates of patients who LWBS during the subsequent 6 hours.
Patient survey
To get the patient’s perspective, we conducted a prospective study with a sample of recently registered patients to determine their expectations regarding ED wait times. A follow-up phone call at 1 week assessed their opinions of care received, global satisfaction levels, and suggestions for improvement. Patient data were collected for 3 weeks in the summer and 6 weeks in the fall of 2003 to reach an enrollment goal of 300. Research assistants (RAs) were trained to use a verbal script for survey administration, and they were supervised by the primary author.
Noncritical adult patients between the ages of 18 and 65 years were approached consecutively in reverse regis- tration order during a convenience sample of 40 evening shifts. With 1 research assistant per shift, not all eligible patients were approached. In the likely event that more than 1 eligible patient was waiting, the most recently registered was approached for survey participation. Because prior analysis determined that LWBS rates are higher in the evening, we enrolled patients arriving after 4:00 pm to increase the likelihood of capturing more LWBS patients. Patients were excluded if they were too sick to remain in the waiting room or were directly admitted by ambulance, were sleeping or unable to converse with the interviewer, or did
not respond when their name was called. The initial patient survey, administered in written or verbal format depending on patient preference, collected demographic data, health care sources, reasons for visit, wait time expectations, and suggestions for improving ED care.
The follow-up patient survey was a scripted phone questionnaire given to enrolled patients within 1 to 3 weeks of the initial visit. We considered an enrolled patient lost to follow-up only if we were unable to contact them after
5 phone attempts during different times of the day and week. One important goal of this study was to understand health outcomes of patients not remaining for treatment. Therefore, LWBS patients were asked whether they had sought alternative care or whether their problem had resolved without treatment. They were also asked how long they waited before LWBS, what were their reasons for leaving, and what might have prevented their leaving. Patients who remained for treatment were also asked what their wait times had been, along with an assessment of quality, satisfaction, problem resolution, and adherence to recommended follow-up. Recommendations for improving ED care and any additional comments were also solicited.
Data analysis
All statistical analyses were performed using Stata 7.0 (Stata Corporation, College Station, Tex). The administra- tive data were described using percentages or means. The LWBS characteristics of different subgroups were analyzed using the v2 test, with differences deemed significant if P b.05. We evaluated the strength of these associations with a Relative risk .
For the ED provider crowding assessments, we used a weighted Cohen’s j calculation to test agreement on crowding and compromised care. Providers were considered in close agreement if they selected within 1 point of each other and we selected weights accordingly. Therefore, Likert assessments that were exact and within 1 unit were weighted
1.0 and 0.9, respectively. All assessments more than 1 unit away were weighted 0.0. We judged agreement as almost perfect if j N 0.80, substantial if 0.61 z j V 0.80, moderate if 0.41 z j V 0.60, fair if 0.21 z j V 0.40, slight if 0.00 z j V 0.20, and less than chance if j V 0.00 following Landis and Koch’s frequently cited scale [16].
Patient surveys were analyzed descriptively with percen- tages and means. Variations in patient satisfaction at different levels of perceived wait times were tested using unpaired t tests and v2 tests. Differences were considered significant if P b .05.
Results
Administrative data
Analysis of the January 2003 ED administrative logs identified the characteristics of patients who LWBS com-
pared with those who remained for treatment. These characteristics proved robust for all subsequent data collection periods. Therefore, data from all 4 periods were merged to report overall trends for 11743 patients who registered during data collection periods. Characteristics of all patients compared with those who LWBS vs those who remained are detailed in Table 1. Patients were 65% female; mean age, 43 years; and 9% of the patients LWBS.
Patients were more likely to LWBS if they were young (v2, P b .001), had no insurance (v2, P b .001), or were triaged to the green (highest nonurgent) and orange (stable urgent) categories (v2, P b .001). Patients younger than 45 years had an LWBS RR of 1.7 (95% confidence interval [CI], 1.5-1.9) vs those older than 45 years. patients without insurance had an LWBS RR of 1.5 (95% CI, 1.3-1.7) compared with those with private insurance, Medicare, or Medicaid. However, because a greater portion of our patients had some form of insurance coverage, 74% of all patients who LWBS were insured, and 28% of these had private insurance. Of patients who LWBS, 90% had been triaged as nonurgent or stable (blue, green, or orange), whereas only 77% of arriving patients were triaged with these acuities (RR = 3.1; 95% CI, 2.5-3.8).
Patients in the emergent and potentially unstable urgent categories also LWBS; 6 patients who were triaged as emergent (red) and 87 triaged as potentially unstable (yellow) LWBS over the study period. Twenty-one patients older than 80 years left without being seen during the study period even though patients older than 80 years were
3.3 times more likely to be classified as urgent or emergent
Table 1 All patients registering during the 4 data collection
periods: total and LWBS vs remained for treatment (data from ED registration log)
Data are expressed in percentage unless otherwise stated.
|
Total, n = 11743 |
LWBS, n = 1081 |
Remained for treatment, n = 10662 |
|
|
Mean age (y) |
43 |
38 |
44 |
|
Sex |
|||
|
Men |
35 |
32 |
35 |
|
Women |
65 |
68 |
65 |
|
Race |
|||
|
Black |
91 |
93 |
91 |
|
White/other |
9 |
7 |
9 |
|
Medicaid |
31 |
33 |
31 |
|
Medicare |
21 |
13 |
21 |
|
Private |
29 |
28 |
30 |
|
None |
19 |
26 |
18 |
|
Acuity Red |
8 |
1 |
9 |
|
Yellow |
15 |
8 |
16 |
|
Orange |
25 |
31 |
24 |
|
Green/blue |
52 |
60 |
51 |
|
LWBS |
9 |
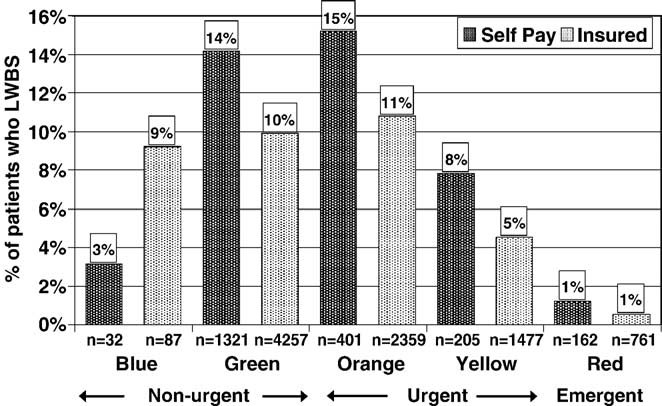
Fig. 1 Percentage of patients who LWBS by insurance status and acuity. Self-pay patients were more likely to LWBS when triaged to the orange category, that is, needs medical attention but is stable to wait. This category experiences the longest wait times on average.
than those younger than 30 years (v2, P b .001). Finally, of our uninsured patients, those in the stable urgent (orange) category left at the highest rates (15%) and were 1.4 times more likely to LWBS than those of similar acuity with insurance (v2, P b .010) (Fig. 1). There were also day-of- the-week and time-of-day variations in rates of LWBS. In particular, patients LWBS 1.4 times as frequently from Monday through Wednesday than during the remainder of the week (v2, P b .001). In addition, patients were 2.4 times more likely to LWBS during night shifts, defined as 6:00 pm to 6:00 am (v2, P b .001).
Provider survey
There were 35 6-hour periods out of a total of
57 analyzed in which either the attending physician or charge nurse on duty deemed the ED to be crowded. Over the study period, when the charge nurses perceived that the ED was crowded, they felt care was compromised 48% of the time and they were uncertain 26% of the time. When the physicians perceived that the ED was crowded, they felt care was compromised 70% of the time and they were uncertain 15% of the time. There was a significant level of consensus between the attending physician and the charge nurse working the same shift as to whether the ED was crowded (81% agreement, j = 0.537). Notably, LWBS rates correlated well with provider perception ( P b .01), rising as the provider rating of crowded conditions in- creased (Fig. 2).
Although the attending physician and charge nurse had consensus on level of crowding, using the same measure- ment scale, they did not always agree on exactly when care was compromised (54% agreement, j = -0.003). There were 14 shifts when the attending physician felt the ED was crowded and care compromised and 15 shifts in which the charge nurse felt this way. However, in only 2 of 27 shifts were the 2 providers in agreement, meaning that 27 (47%) of 57 of the time, at least 1 of the 2 key ED providers felt
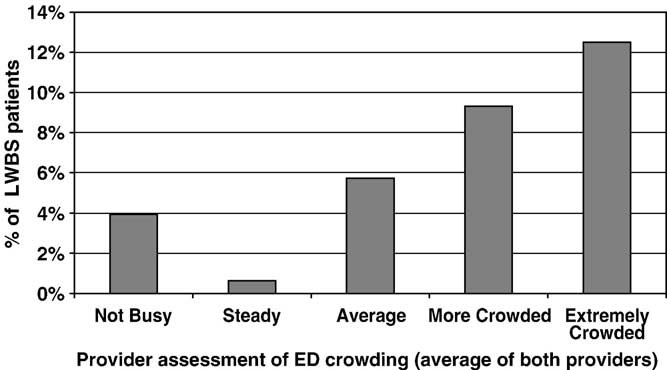
Fig. 2 Percentage of patient who LWBS during varying levels of perceived crowding by providers. Once the providers have perceived that the ED census has elevated into a crowded state (average to extremely crowded), there is a positive correlation between the level of crowding and the percentage of patients who LWBS.
that crowding was compromising the quality of patient care and possibly jeopardizing patient safety.
Patient survey
A total of 890 potentially eligible patients arrived in the ED during data collection periods. Because of limited RA time in the ED and the length of time required to administer the survey, we were able to approach 423 patients; of these, 310 (73%) enrolled and completed the
Fig. 3 Study flow diagram for patient expectations and follow- up Satisfaction surveys.
initial survey (72% female; mean age, 36 years; 9% LWBS). Of the enrolled patients, 174 (56%) of 310 were reached for the follow-up survey (76% female; mean age, 36 years; 11% LWBS) (Fig. 3). In Table 2, the characteristics of patients who completed the follow-up are compared with those who did not.
Although believing the appropriate wait time for ED care to be less than 1 hour, patients expected an average wait of
2.1 hours, higher if they had experience with our ED. Waits over 5 hours were expected by 14% of the patients. Actual wait times reported by the patients averaged 3.5 hours. Satisfaction with the perceived wait times decreased significantly if waits exceeded 1 hour and were very low after 4 hours (ratings: 4.1, 2.6, 1.6, respectively, using a 1 [low] to 5 [high] Likert scale, v2, P b .001).
Most patients seen were satisfied with the quality of medical care received once seen by a physician. However, overall visit satisfaction dropped significantly when the perceived wait exceeded 4 hours (3.8 vs 2.7, t test, P b
.001). Patients who were most unhappy were in significant pain, bleeding, or felt they were unjustly waiting longer than other patients. The overriding patient suggestion for how to improve ED care was to decrease waiting times.
The average perceived wait of patients who LWBS was reported as 5.1 hours vs a 3.2 average rate reported by patients who remained for treatment (t test, P b .01). Patients reported that they left because the wait was too long
Table 2 A comparison of patient demographics for those
who completed vs those who did not complete the follow-up phone survey
* For age, a 2-sample t test with unequal variances was used to test
if the means of the 2 groups were the same. For the remaining reported categories, a v2 test was used to test if the proportion of patients in the follow-up survey was the same as those who did not. These hypotheses were rejected if P b .05.
|
Completed follow-up, |
No response in follow-up, |
P* |
|
|
n = 174 (56%) |
n = 136 (44%) |
||
|
Mean age (y) |
36 |
36 |
.881 |
|
Sex |
.063 |
||
|
Men |
24 |
33 |
|
|
Women |
76 |
67 |
|
|
Race |
.259 |
||
|
Black |
86 |
91 |
|
|
White/other |
14 |
9 |
|
|
Insurance |
.308 |
||
|
Medicaid |
45 |
37 |
|
|
Medicare |
10 |
7 |
|
|
Private |
29 |
38 |
|
|
None |
15 |
18 |
|
|
Acuity |
.185 |
||
|
Red |
- |
- |
|
|
Yellow |
9 |
5 |
|
|
Orange |
34 |
29 |
|
|
Green/blue |
56 |
66 |
|
|
LWBS |
11 |
7 |
.176 |
(78%), they were too sick to wait (28%), or they felt mistreated by the ED staff (22%). Of the 19 who LWBS,
10 (53%) still had the problem, including 2 who went elsewhere, 10 (53%) went elsewhere, and 1 (5%) got better without care. Of the 7 potentially unstable patients who had LWBS, 4 had not received care elsewhere at the time of follow-up.
Discussion
Our principal findings support the assertion that access, as measured by those who LWBS, and quality, as measured by patient satisfaction, are adversely affected by crowding. Many patients who require urgent and even immediate care are effectively being denied access to that care because of crowded conditions and prolonged waits. If we projected our 13 weeks of administrative results over a full year, we might expect that 365 unstable patients, 310 insured and 1275 uninsured patients requiring medical treatment, 490 patients older than 60 years, and 80 patients older than 80 years would come to our ED, wait for care, and leave before treatment. Almost half of the time, either the attending physician or the charge nurse felt that patient care in our urban academic ED was compromised by crowded conditions. Although they had very different periods of discomfort, providers were in substantial agreement in their assessments of crowded conditions, and these assessments were highly associated with increased rates of patients who LWBS. Finally, although our urban, predominantly African American patients valued the care they received and expected to wait several hours to be seen if presenting with a nonurgent condition, patient perceived ED wait times that exceeded 4 hours negatively impacted both the perceived quality of care and the rates of LWBS.
In the last decade, there has been a 33% growth in wait times and a tripling of the numbers of patients who LWBS by a physician, particularly in large metropolitan areas [1]. Ambulance diversion, the process of diverting emergency vehicles away from the closest, but overwhelmed, ED, has also become increasingly common, with 1 in 20 hospital EDs being on diversion at least 20% of the time [4]. In a national survey of ED directors, 37% said patients had excessive waits. In fact, 67% of these physicians believed that patients were at risk for poor health outcomes and 33% reported poor health outcomes directly attributable to ED crowding [17]. Others have investigated the negative impact of crowding on Quality of ED care. Schull et al [18] documented this in a study linking ED crowding to delay in thrombolysis for patients with suspected acute myocardial infarctions, and Bernstein et al [19] used an ED work index to quantitatively test the relationship between ED crowding and adverse events.
Baker et al [13] found that 46% of those who LWBS were identified as needing prompt medical evaluation. Of patients who LWBS, 11% were subsequently hospitalized,
and 4 developed riskier health conditions requiring more extensive and expensive care because of the delay. Similarly, Bindman et al [20] determined that 49% of their LWBS patients were classified as needing care within 3 hours, 28% returned to an ED, and 5% were hospitalized within 2 weeks. In their study, 1 patient developed a Serious condition because of the Delay in care.
We also had several concerning findings with our patients who LWBS. In total number, most patients who LWBS were insured, consistent with our first hypothesis that those patients with increased resources would be more likely to LWBS. However, patients without insurance, who frequently lack other opportunities for medical care, left at a higher rate particularly in the stable urgent (orange) category. Of our LWBS patients contacted on follow-up, only 1 of 19 got better without further care. Of the remainder, 10 (53%) sought care elsewhere subsequently:
- at another ED and 3 at a primary care facility. However,
- (42%) patients were still experiencing the problem that had brought them to the ED.
Consistent with Bullard et al [21], we found elderly patients less likely to LWBS than young patients. However, in our 13 weeks of study, 21 patients older than 80 years left the ED without being seen by a physician. In the elderly, a protracted health problem can quickly affect ongoing quality of life or lead to increased mortality. Although patients assigned to nonurgent triage categories are likely to have good health outcomes even if they leave, the situation for patients in the urgent (orange or yellow) categories is less clear. These patients are at higher risk for adverse health outcomes. Our policy is to see emergent patients within
30 minutes, if not immediately. The potentially unstable (yellow) must be reevaluated within 2 hours. In the main ED, patients are brought back in order of acuity and then arrival, so our urgent stable patients will be seen after patients of higher acuity. At the same time, our stable (blue/ green) patients can be seen in a fast-track area at a faster rate. This results in the urgent stable patient waiting the longest, likely a reason they are the group with the highest LWBS rates. At least 2 participants in our survey triaged to the orange category ultimately were hospitalized after spending over 7 hours in the waiting room. Finally, of greatest concern, 6 patients assessed as emergent and needing immediate care left without receiving medical attention. One of these patients was a 75-year-old woman with chest pain and another was short of breath. The remaining 4 patients who LWBS were triaged as having emergent psychiatric issues; 1 was suicidal by chief complaint. The lack of prompt attention for these patients could have had serious consequences for themselves or others.
As reported in the literature, providers readily recognize when the ED is crowded. The impact of this crowding on quality of care is not as clear. It is concerning that, in 47% of the shifts we studied, at least one of the providers felt that the quality of care was compromised by crowded con- ditions. Curiously, nurses and doctors tended to disagree on
exactly when care was compromised. It is possible that compromised care is not easily measured, or that the definition varies for different providers at different times. For example, we have previously found that crowded conditions in our ED are highly associated with the number of bboarded patients,Q that is, already admitted patients awaiting an inpatient hospital bed who are being cared for by the ED staff [22]. It would not be surprising to find that once a sick patient in need of admission has completed his/ her diagnostic evaluation, physicians are free to see new patients, whereas nurses still need to continue to provide care as long as the patient remains in the ED. Thus, it is possible that the presence of boarded patients dispropor- tionately compromises the quality of nursing care and could explain the discrepancy in the timing of compromised care evaluations between attending physicians and charge nurses. However, the current study was not designed to answer that question. Consistent with our second hypothesis, although providers did not agree on whether care was compromised, access as measured by LWBS rates was highly correlated with provider ratings of crowding.
Although our patients believed care should be received within 1 hour, they expected to wait at least twice that long at our academic urban ED. As described by Green et al [23], length of stay is significantly correlated with LWBS rates. Our study shows that when patients believe their waits extend beyond expectations, it impacts the perceived quality of the medical care received. Both of these factors could impact patients’ willingness to pursue emergency care in the future.
Limitations
These results have several important limitations. They come from 1 academic ED, which may or may not be generalizable to other urban academic settings. In addition, we deliberately performed the survey in evening hours because we were most interested in capturing LWBS patients. Overall, nighttime ED patients may not be representative of all patients. Although an attempt was made to representatively sample administrative data from all 4 seasons, sampling does not capture all adverse events. Our patient follow-up sample was small, and even with a 73% consent rate, we were only able to capture 35% of potentially eligible patients who presented during data collection periods. Therefore, patients who were missed or elected not to participate may have had very different wait time experiences and rates of satisfaction. Likewise, we were able to capture specific concerning issues from our surveyed patients who LWBS; however, we recognize that these 19 patients are a small fraction of our LWBS population. Lastly, our data on the wait times of patients, particularly of those who LWBS, were self-reported and may not reflect the actual wait times. Our administrative log reports only times of arrival and departure for those patients
who are treated and discharged from the ED. The patient- reported wait times are consistent with these overall patient stay times, as well as with those of patients who did not LWBS. However, it is recognized that this is not a strong corroboration of reported waits.
In retrospect, capturing actual patient wait times and correlating these findings with perceived waits and LWBS rates would have enhanced our findings. In addition, it would be informative had we been able to compare patient and provider perceptions of when care is compromised. Overall, this is a small multimethod single-site study that nonetheless serves to raise some intriguing hypotheses, which will need to be tested further in a multisite study.
Conclusion
We found evidence that ED crowding, which results in extended wait times and high rates of patients who LWBS, functionally restricts access to emergency services and compromises the quality of care as perceived by patients and providers. In our study, the impact of restricted ED access fell disproportionately on those who lack other health care options. However, even insured patients who waited and finally received care did so after extended suffering or frustration. Although this situation may or may not have hindered the Healing process, no one would regard it as high quality emergency care. If these results are generalizable, systemwide changes in the organization of acute care will be necessary for the ED to fulfill its role as a safety net provider and meet public health needs for surge capacity in the event of disasters.
Acknowledgments
The authors thank Brent Asplin, MD, who contributed to the study design and provided feedback on earlier drafts of the manuscript, the Pritzker Summer Research program, and the research assistants, faculty, nurses, residents, staff, and patients at the University of Chicago Emergency Medicine Program, Chicago, IL.
References
- Bitterman RA. Explaining the EMTALA paradox. Ann Emerg Med 2002;40:470 - 5.
- Clancy CM, Eisenberg JM. Emergency medicine in population-based systems of care. Ann Emerg Med 1997;30:800 - 3.
- McCaig LF, Burt CW. National Hospital Ambulatory Medical Care survey: 2003 emergency department summary. Advanced data from vital and health statistics; no. 358. Hyattsville (Md)7 National Center for Health Statistics; 2005.
- U.S. General Accounting Office. Hospital emergency departments: crowded conditions vary among hospitals and communities. Wash- ington (DC)7 GAO; 2003.
- Kellermann AL. De’ja` Vu. Ann Emerg Med 2000;35:83 - 5.
- Derlet RW, Richards JR. Overcrowding in emergency departments: complex causes and disturbing effects. Ann Emerg Med 2000;35:63 - 8.
- Title 42, Chapter 7, Subchapter XVIII, Sec 1395dd. US Code Collection. LII legal information institute. Available at: www4.law. cornell.edu/uscode/42/1395dd.html. Accessed March 2003.
- Weissman J. Uncompensated hospital care: will it be there if we need it? JAMA 1996;276:823 - 8.
- Schafermeyer RW, Asplin BR. Hospital and emergency department crowding in the United States. Emerg Med 2003;15:22 - 7.
- Kennedy J, Rhodes KV, Walls C, Asplin B. Access to emergency care: restricted by long wait times and cost/coverage concerns. Ann Emerg Med 2004;43:567 - 73.
- McCaig LF, Ly N. National Hospital Ambulatory Medical Care survey: 2000 Emergency Department summary. Advanced data from vital and health statistics; no 326. Hyattsville (Md)7 National Center for Health Statistics; 2002.
- University of Chicago Hospitals, Section of Emergency Medicine, Internal Report, Subject: ED data. May 28, 2003.
- Baker DW, Stevens CD, Brook RH. Patients who leave a public hospital emergency department without being seen by a physician. Causes and consequences. JAMA 1991;266:1085 - 90.
- Hobbs D, Kunzman SC, Tandberg D, Sklar D. hospital factors associated with emergency center patients leaving without being seen. Am J Emerg Med 2000;7:767 - 72.
- Asplin D, et al. Measuring emergency department crowding and hospital capacity [abstract]. Acad Emerg Med 2002;9:366 - 7.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159 - 74.
- Derlet RW, Richards JR, Kravitz RL. Frequent overcrowding in U.S. emergency departments. Acad Emerg Med 2001;8:151 - 5.
- Schull MJ, et al. Emergency department crowding and thromboly- sis delays in acute myocardial infarction. Ann Emerg Med 2004;44: 577 - 85.
- Bernstein SL, et al. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med 2003; 10:938 - 42.
- Bindman AB, Grumbach K, Keane D, Rauch L, Luce JM. Consequences of queuing for care at a public hospital emergency department. JAMA 1991;266:1091 - 6.
- Bullard MJ, Holroyd B, Craig W, et al. Patients who leave without being seen in the emergency department [abstract]. Acad Emerg Med 2000;8:576 - 7.
- Asplin BR, Magid DV, Rhodes KV, et al. A conceptual model of emergency department crowding. Ann Emerg Med 2003;42: 181 - 4.
- Green RA, Wyer PC, Giglio J. ED walkout rate correlated with ED length of stay but not with ED volume or hospital census [abstract]. Acad Emerg Med 2002;9:514.
