Magnetic resonance imaging and computed tomography utilization trends in an academic ED
a b s t r a c t
Objective: The objective of this study is to examine the annual utilization trends of emergency department (ED)- orderED magnetic resonance imaging (MRI) and computed tomography (CT) at an urban academic hospital from 2007 to 2011. We hypothesized that MRI and CT use would increase annually over the study period.
Methods: This was a retrospective observational study of ED encounters between January 1, 2007, and December 31, 2011. All patients seen by a provider were identified, and demographics were abstracted. Type of CT and/or MRI examination, clinical indication, and final disposition were collected. Records of patients with an ED-ordered MRI were also examined for presence of a CT within +-3 days of their encounter date. Unadjusted linear regression was used to assess for differences among years for both CT and MRI. Secondary outcomes were descriptively summarized.
Results: A total of 7089 MRI (20 per 1000) and 85673 CT (243 per 1000) examinations were ordered over a 60- month period. Computed tomography use decreased significantly (P = .021). Magnetic resonance imaging use significantly increased (2.2 per 1000 ED visits each year, P = .005). Magnetic resonance imaging of the head was ordered most frequently (10.7 per 1000). The overwhelming majority of MRI images were completed for acute neurologic/behavioral problem. Of patients with an MRI completed, 89.4% had a CT completed within 3 calendar days with most of the CT examinations (81%) completed during the encounter.
Conclusion: There was a steady increase in MRI testing in our academic ED, with most MRIs ordered for acute neurologic or behavioral changes. There was a corresponding decreasing trend for CT scans.
(C) 2014
Introduction
Background
Multiple studies have demonstrated tremendous growth in the use of computed tomography (CT) over the last decade [1-5]. A CT examination can quickly diagnose or exclude many Serious conditions and offer valuable information about organs, vessels, bone, and musculature that plain radiographs, nuclear imaging, or ultrasonog- raphy may miss. In fact, CTs can even diagnose conditions that the physician has not considered. This diagnostic accuracy is seductive to
? Funding was provided by the HealthPartners Institute for Education and Research Internal Grant Program.
?? Author Contributions: KAQ, JGS, and BDG conceived the study, designed the
trial, and obtained research funding. KAQ, JGS, and BDG supervised the conduct of the trial and data collection. JGS and KAQ provided oversight for data analysis; KAQ and JGS drafted the manuscript, and all authors contributed substantially to its revision. KAQ takes responsibility for the article as a whole.
? Presented as an oral presentation at the Great Plains Society for Academic
Emergency Medicine Regional Meeting, September 29, 2012, St. Louis, MO.
?? Conflicts of interest: None.
* Corresponding author. Regions Hospital, 640 Jackson St, MS 11109F, St Paul, MN 55101. Tel.: +1 651 254 5302; fax: +1 651 254 5314.
E-mail address: [email protected] (J.G. Salzman).
emergency department (ED) physicians who have limited time and information in which to make decisions regarding treatment and disposition. Unfortunately, this diagnostic tool comes at a cost in the form of radiation exposure. There is growing concern that the future may show a rise in malignancies related to diagnostic imaging [6-8]. Brenner and Hall [6] have recently predicted that 1.5% to 2% of all cancers in the United States may be related to radiation exposure from CT scans. Miglioretti et al [7] reported “Nationally, 4 million pediatric CT scans of the head, abdomen/pelvis, chest, or spine performed each year are projected to cause 4870 future cancers.” Sodickson et al [8] estimate that CT exposures “produced 0.7% of total expected baseline cancer incidence and 1% of total cancer mortality.” The risk of radiation exposure and potential for future Negative outcomes require ED physicians to balance these concerns with a need to optimize care in an emergency setting.
One alternative to CT is magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA). These examinations offer excellent visualization of most organs without radiation. Magnetic resonance imaging examinations generally take longer and are usually performed at locations remote from the ED, where unstable patients would be inappropriate. Magnetic resonance imaging also may not be appropriate for some patients due to claustrophobia and/ or retained metal or implants. Despite these constraints, MRI may be
http://dx.doi.org/10.1016/j.ajem.2014.01.054
0735-6757/(C) 2014
an option for many emergency patients. Studies have demonstrated appropriate roles for emergent MRI studies, including the evaluation of stroke, transient ischemic attack, pulmonary embolism, Spinal cord compression, appendicitis, Cardiovascular emergencies, and Trauma victims [9-16]. For some conditions, MRI offers more diagnostic accuracy than CT. Yet, to date, there is limited evidence that there has been an increase in MRI use for emergency patients [17-19].
Importance
Magnetic resonance imaging use in academic EDs is poorly understood. With evidence that MRI may be an alternative to CT, understanding actual usage patterns in this setting would help generate additional questions regarding appropriate use of this tool and whether MRI use has any impact on use of other diagnostic imaging tools (CT or ultrasound). With a focus nationwide on optimizing Patient care and safety through evidence-based evalua- tion, best practices would suggest that reducing radiation and unnecessary testing are key strategies. Understanding current utilization trends allows for defining best practices associated with MRI use in an emergency setting.
Goals of this investigation
The primary aim of this study was to describe the annual utilization trends of MRI and CT imaging ordered in an ED at a single urban academic hospital over a 5-year period (2007-2011). These utilization trends were normalized to the number of tests per 1000 encounters. We hypothesized that MRI and CT use would both increase annually over the 5-year study period.
Secondary aims of this project included evaluation of the types of CTs and MRIs ordered over this period, the chief complaints associated with these imaging orders, and a descriptive evaluation of the concurrent use of CT and MRI on the same patient by anatomical location.
Materials and methods
Study design
This project used a retrospective Observational study design. The HealthPartners Institutional Review Board reviewed and approved the study.
Setting and selection of participants
The study was performed using records from all emergency visits to our Urban academic ED between January 1, 2007, and December 31, 2011. Our hospital is a 425-bed facility designated as a primary stroke center, a level I adult and pediatric trauma center, and a verified Burn center. Computed tomography and MRI are available 24 hours a day with immediate reading by board-certified radiologists. During the study period, MRI had on-site staff available to complete studies for both day and evening shifts (0700-2300) and was also available in an on-call fashion for emergency studies during night shifts (2300-0700).
All patients, regardless of age, registered and seen by a provider in the ED between January 1, 2007, and December 31, 2011, were evaluated through hospital billing and radiology systems for inclusion into the study. Patients listed in the organization’s research opt-out registry and those without an MRI or CT ordered in the ED were excluded.
Methods of measurement
After identification of eligible patients, a research informatics specialist extracted the following data elements for each patient: (1)
age, (2) sex, (3) mechanism of injury, (4) chief complaint, (5) type of CT or MRI/MRA examination, (6) clinical indication documented by provider for the evaluation, and (7) final disposition. Magnetic resonance angiography was included with MRI. Similar data were also obtained for CT and included CT angiography. Multiple MRI studies for an individual patient were counted separately. When there was more than 1 type of Imaging study conducted for an anatomical location (eg, Head CT.with and without contrast), each imaging study was counted separately. Clinical indications are chosen by the ordering provider from a drop-down menu in the electronic medical record. Indications, chief complaints, and image orders were consol- idated into broad categories based on consensus of the investigators. Each patient’s electronic medical records were screened for CT done within 3 days before or after the date of an ED visit where an MRI was completed. The anatomical type of CT was noted.
Data collection and processing
Data were electronically abstracted by research programming analyst and provided to the study investigators in summary format. To ensure appropriate data extraction, one of the investigators (KAQ) independently reviewed 20 patient records against the data extracted by the programming staff. This quality assurance measure resulted in 100% verified data points.
Primary data analysis
An unadjusted linear regression model was used to assess for difference among years for both CT and MRI rates. Our secondary outcomes were descriptively summarized.
Results
Characteristics of study subjects
Over the 5-year study period, 360662 patients had records created at our hospital. Five hundred eleven patients were excluded due to their name listed on our organization’s opt-out registry. An additional 3756 records were excluded for registering but not being seen by a provider, leaving 356395 patients for review. Table 1 shows ED census and demographic statistics as well as the total number of ED- ordered MRI and CT examinations by year from 2007 to 2011. Between 2007 and 2011, there was a 20% increase in the annual census numbers, with the proportion of pediatric patients (9.29%- 10.63%), the percentage presenting with trauma (16.72%-19.06%), and admission/transfer rate (23.07%-24.26%) remaining relatively stable.
Main results
A total of 7089 MRI and 85673 CT examinations were ordered in the ED over a 60-month period, resulting in an average of 20 MRIs and
243 CTs per 1000 ED patient visits. Computed tomography use decreased significantly over the 5-year period (P = .021), with a predicted decrease of 13.6 per 1000 annually. Magnetic resonance
Table 1
Overall department utilization statistics per year
|
2007 |
2008 |
2009 |
2010 |
2011 |
|
|
Total ED census |
64817 |
66721 |
70787 |
75922 |
78148 |
|
Admission rate (%) |
23.07 |
24.26 |
24.16 |
24.07 |
23.75 |
|
No. of MRIs ordered |
1003 |
1151 |
1423 |
1665 |
1847 |
|
No. of CTs ordered |
16757 |
17776 |
17432 |
17321 |
16387 |
|
No. of MRIs per 1000 visits |
15.47 |
17.25 |
20.10 |
21.93 |
23.63 |
|
No. of CTs per 1000 visits |
258.53 |
266.42 |
246.26 |
228.14 |
209.69 |
|
Total (%) pediatric (0-17 y) |
10.63 |
9.29 |
10.43 |
9.40 |
9.62 |
|
Total (%) trauma |
19.06 |
18.51 |
17.42 |
17.88 |
16.72 |
imaging use significantly increased over the study period, with an increase of 2.2 per 1000 ED visits each year (P = .005).
Table 2 shows the demographics of patients who had MRI ordered in the ED as well as the anatomical grouping categories of MRIs completed. Table 3 demonstrates the same for patients who had a CT ordered in the ED during this 5-year period. Trauma patients had a CT ordered more frequently than an MRI. Patients who had MRI or CT imaging were admitted or transferred approximately 50% of the time, which is twice the average ED Population rate. Magnetic resonance imaging of the head was ordered most frequently (10.7 per 1000), followed by MRA neck (2.9 per 1000), MRI lumbar spine (2.2 per 1000), MRI cervical spine (2.0 per 1000), and MRI extremity (0.83 per 1000). Computed tomography was done primarily of the head, abdomen, and cervical spine during this time.
The overwhelming majority of MRI images were completed for acute neurologic/behavioral problem, with trauma being the second most common reason (Table 4). Table 5 lists the top 5 indications for each type of CT. Trauma was the leading indication for CT imaging, with acute neurologic/behavior problem coming in a distant second. A total of 6339 patients (89.4%) had CT done within 3 calendar days of an ED visit with MRI ordered. Most of these CT examinations (81%) were done during the ED visit where an MRI was done. Only 5% had CT done in the 3 days before an ED visit, and 14% had a CT done after being seen in the ED. These CT examinations were not necessarily of the same anatomical region. Of all patients who had both during a 3-day period, 2899 (45.7%) were for the same anatomical location. When duplicate imaging (CT and MRI) was performed of the same anatomical location, it was primarily done of the head/brain (76.4%) and 13.4% of the time for the cervical spine
(Fig.). All other sites combined accounted for 10% of studies.
Table 3
Distribution of demographics and patient characteristics who had ED-ordered CT
|
2007 |
2008 |
2009 |
2010 |
2011 |
|
|
Male (%) |
56.45 |
57.21 |
56.48 |
53.74 |
53.98 |
|
Trauma (%) |
42.82 |
37.93 |
35.26 |
34.92 |
34.34 |
|
b18 years of age (%) |
7.34 |
5.5 |
5.54 |
4.9 |
4.26 |
|
N 64 years of age (%) |
20.3 |
22.32 |
21.41 |
23.04 |
23.87 |
|
CT head |
6494 |
9587 |
6668 |
6793 |
6680 |
|
CT neck |
248 |
302 |
345 |
402 |
486 |
|
CT cervical spine |
2223 |
2356 |
2292 |
2348 |
2258 |
|
709 |
842 |
753 |
709 |
602 |
|
|
CT lumbar spine |
830 |
908 |
844 |
814 |
732 |
|
CT abdomen |
5022 |
4986 |
4301 |
3974 |
3599 |
|
CT extremities |
193 |
243 |
200 |
203 |
209 |
|
Admitted (%) |
53.34 |
57.09 |
56.14 |
53.97 |
54.69 |
not necessary. We also did not investigate if patients had an MRI done after leaving the ED as an inpatient or outpatient.
5. Discussion
The literature is replete with studies demonstrating a rise in CT use in this country, provoking many physicians to reconsider use of this modality [1-5]. Alternatively, there are only a few studies on utilization trends of MRI in EDs. Rankey et al [17] reviewed a single academic medical center data from 2001 to 2005 for MRI examina- tions ordered in the ED. They found an increase of 38.9% despite a decline in total ED volume during this period. Their mean MRI
Table 4
Top 5 clinical indications for ED-ordered MRI examinations, 2007 to 2011
1 2 3 4 5
4. Limitations
This study has several limitations. First, it involves a single academic center in a large Midwestern metropolitan area and may
MRI head Acute neuro/ behav problem (2700)
Weakness (154)
CV
problem (139)
Trauma (121) GI concern
(106)
not be comparable with other institutions. Residents and fellows may have been the ordering provider, but these tests are rarely done without direct approval of supervising emergency medicine board- certified staff physicians. It also is a Tertiary trauma center with a high
MRI neck Acute neuro/ behav problem (693)
Trauma (48)
CV
problem (38)
Weakness (36)
Neck/back pain (26)
percentage of blunt traumas, which may have increased the amount of
CT and MRI imaging. Second, this study’s retrospective nature prevents understanding the thought processes that led to a decision to order an MRI for any given patient. Indications were reviewed but may not fully reflect the situation as they were part of a drop-down menu. The hospital has guidelines involving CT examinations for clinical conditions like stroke and trauma, but there are no institution- specific guidelines or order sets for MRI examinations. Indications were available from a drop-down menu on the electronic medical record. Third, this study cannot comment on the true necessity of the MRI examinations ordered. It is possible that some of these tests were
Distribution of demographics and patient characteristics who had ED-ordered MRI
2007 2008 2009 2010 2011
MRI
cervical spine
MRI
thoracic spine
MRI
lumbar spine
MRI
abdomen
|
(14) |
(4) |
||||
|
MRI |
Extremity |
Trauma |
Acute |
Skin problem |
Weakness (6) |
Trauma (287)
Trauma (82)
Trauma (100)
Extremity pain (29)
Neck/ back pain (152)
Acute neuro/ behav problem (34)
Extremity pain (100)
GI
concern
Acute neuro/ behav problem (116)
Neck/ back pain (14)
Acute neuro/ behav problem (85)
Trauma (14)
Extremity pain (38)
Extremity pain (14)
Miscellaneous/ other/ unknown (22)
Acute neuro/ behav problem
Miscellaneous/ other/ unknown (15)
Weakness (11)
Weakness (20)
CV problem (3)
|
Male (%) |
49.25 |
44.48 |
42.16 |
47.15 |
47.7 |
extremities |
pain |
(50) |
neuro/ |
(7) |
|
Trauma (%) |
16.55 |
13.38 |
14.9 |
14.53 |
14.51 |
(157) |
behav |
|||
|
b18 years of age (%) |
3.49 |
3.04 |
4.01 |
3.14 |
1.68 |
problem |
||||
|
N 64 years of age (%) |
20.84 |
23.46 |
26.14 |
26.55 |
25.5 |
(30) |
||||
|
MRI head |
510 |
636 |
828 |
880 |
986 |
MRI chest |
Chest |
Acute |
CV |
Weakness, |
|
MRA neck |
155 |
160 |
206 |
236 |
263 |
pain (16) |
neuro/ |
problem |
respiratory |
|
|
MRI cervical spine |
107 |
118 |
128 |
157 |
198 |
behav |
(2) |
problem, ENT |
||
|
MRI thoracic spine |
33 |
34 |
42 |
74 |
77 |
problem |
problem, |
|||
|
MRI lumbar spine |
102 |
128 |
128 |
215 |
233 |
(3) |
hypotension/ |
|||
|
MRI abdomen |
14 |
24 |
27 |
37 |
31 |
shock (1) |
Abbreviations: neuro, neurologic; behav, behavioral; CV, cardiovascular; GI, gastrointestinal; ENT, ears, nose, and throat.
|
MRI extremities |
78 |
45 |
61 |
57 |
54 |
|
Admitted (%) |
47.65 |
47.09 |
49.4 |
50.33 |
51.76 |
Top 5 clinical indications for ED-ordered CT examinations, 2007 to 2011
|
1 |
2 |
3 |
4 |
5 |
|
|
CT head |
Trauma (14597) |
Acute neuro/ behav problem (11449) |
CV problem (1255) |
ENT problem (909) |
Weakness (754) |
|
CT neck CT cervical |
ENT problem (559) Trauma |
Acute neuro/ behav problem (366) Acute |
Trauma (292) Neck/back |
Neck/back pain (121) Extremity |
Respiratory problem (110) CV problem |
Although the MRI utilization rate rose an average of 2.2 per 1000 patient visits (52% over 5 years), we were surprised to find that the utilization rate of CT declined an average of 12 per 1000 patient visits (15% over 5 years). Other studies have shown a rise in CT use, but most of these ended before this period began [2-5]. We believe that this is one of the first studies demonstrating a decline in ED-ordered CT imaging. Because of the more recent years that we reviewed, our results may better represent the current trends in CT use nationally, as efforts to raise awareness of the radiation risks and encourage physicians to use CT judiciously have had time to take effect.
The real dilemma is the uncertainty of optimal utilization rates for
CT examinations in the ED. Computed tomography offers many diagnostic advantages to the ED physician, including increased
spine
CT thoracic spine
CT lumbar spine
CT
abdomen/ pelvis
CT
extremities
(8590)
Trauma (2976)
Trauma (3228)
Trauma (3302)
Trauma (519)
neuro/
behav problem (1203)
Acute neuro/ behav problem (101)
Acute neuro/ behav problem (122)
Abdominal/ pelvic pain (2282)
Extremity pain (443)
pain (353)
Extremity pain (67)
Extremity pain (88)
GI concern (1876)
Acute neuro/ behav problem (9)
pain (251)
Neck/back pain (45)
Neck/back pain (40)
Chest pain (1132)
GI concern (9)
(224)
Chest pain (28)
Miscellaneous/ other/ unknown (33) (next is chest pain, 28) Respiratory problem (760)
Miscellaneous/ other/ unknown (8) (next is CV problem and follow-up, both 7)
certainty, detection of other conditions, and a sense of protection against litigation. It is noteworthy that the rise in CT use in this country happened concurrently with the relative abandonment of other common ED-ordered tests such as intravenous pyelography and nuclear studies for pulmonary embolism or mesenteric vascular disasters. It also coincides with Surgical consultants‘ drive for less negative laparotomies and other operations. These changes have had time to take root, and the testing standards have remained relatively stable over the past few years. Our results may be an accurate reflection of ED physicians’ efforts to balance the need for diagnostic accuracy and the reduction in unnecessary tests and radiation.
The rise in MRI utilization rate was not surprising, but it did not increase as much as we might have expected. If diagnostic accuracy and legal safety nets are drivers for increased CT use, then our institution’s ready access to MRI would suggest that MRI utilization rates should have climbed at an even higher rate. Instead, an annual average rise of 2.2 per 1000 visits seems relatively small compared with the rates of increasing CT utilization published, which vary from 2- to 4.9-fold [2-5].
CT chest Trauma (2249)
Chest pain (1452)
Respiratory problem (1274)
Acute neuro/ behav problem
(290)
CV problem (227)
It is worth noting that the admission rate was nearly double for ED
patients who had a CT and/or MRI than the general ED population. Unfortunately, we did not look at the number of CT or MRI examinations done per patient. Rankey et al [17] noted that patients
CT
chest/ abdomen
Trauma (905)
Chest pain (407)
Acute neuro/ behav problem (115)
Respiratory problem (74)
CV problem (66)
had an average of 1.64 to 1.9 MRI exams per patient. In general, our data would suggest these patients have a higher acuity based on high admission rates. The nature of this review did not permit true assessment of medical necessity.
Our secondary outcomes were related to indications and types of CT and MRI studies done. Most CT images ordered in this period were related to the head, the abdomen, and the cervical spine. The
utilization rate for the ED based on data published was 4.51 per 1000 ED visits. Our results also demonstrate an increase in MRI use in an academic ED each year from 2007 to 2011, but our rate was up to
23.63 per 1000 ED visits. In this study, there were no data published on types of MRI or concurrent use of CT imaging. Raja et al [18] reviewed the 2007 National Hospital Ambulatory Medical Care Survey ED component for head CT and MRI use. They reported 1 in 14 ED patients had a head CT, and 1 in 400 had a head MRI ordered in 2007. The most common reasons for a head CT were trauma, headache, and dizziness. Again, information on the types and indications for MRI exams was not published.
The study by Smulowitz et al [19] reviewed the effect on MRI utilization in a single ED after a large health care insurer mandated preauthorization process for all outpatient CT and MRI studies. There was an increase in MRI ordered in the preauthorization group but also in the control group during the study period between 2003 and 2005. This study did not include patients who were admitted after their imaging and, as such, was limited to only patients who were discharged from the ED and also lacked any information on types of MRI or indications. Our study attempted to describe the MRI utilization rate as well as CT utilization rate for all ED patients at 1 academic trauma center over a more recent period as well as types and indications.
abdominal CT was the only one to have a noticeable decline in utilization over this period. This may reflect a movement toward more bedside ultrasound (Focus Assessment with Sonography for Trauma)
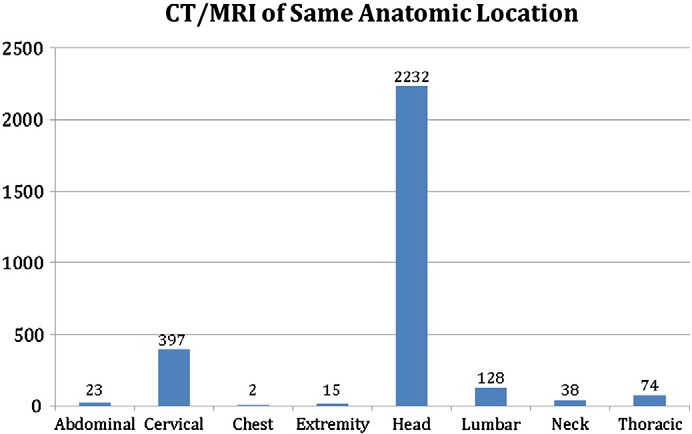
Fig. Comparison of MRI with CT done +-3 days for the same anatomical location, 2007 to 2011; bar graph with vertical axis, the number of examinations. The horizontal axis has groupings of CT/MRI by anatomic location.
for trauma patients in combination with observation. Our findings are similar to others reported in the literature, which have shown an increase in the use of bedside ultrasound and a decrease in the use of abdominal CTs [20,21]. In addition, ultrasounds may also be used in the evaluation of abdominal pain of the pediatric patient in an effort to reduce cumulative radiation doses [22]. A study of CT utilization in a pediatric emergency department from 2003 to 2010 reported a stable rate of abdominal CT utilization rate for abdominal pain but a significant increase in Abdominal ultrasound for abdominal pain [23]. The most common indications for CT imaging were trauma and acute neurologic/behavioral problem, which seems consistent with the types of imaging ordered. It is also comparable with other studies of commonly ordered CT scans in the ED. Of interest, CT of neck (soft tissue and cervical spine) did increase each year. This finding is not surprising and likely a reflection of practice changes nationwide regarding the role of CT in evaluation of cervical spine injury. A meta-analysis published in 2005 found pooled sensitivity of 52% for plain radiographs vs 98% for CT scans in the identification of Cervical spine injuries [24]. In 2009, Eastern Association for the Surgery of Trauma guideline recommended the use of cervical spine CT preferentially to Plain radiography for evaluation of
cervical Spinal injury due to trauma [25].
The clear majority of MRI examinations were of the head, cervical spine, and lumbar spine and MRA of the neck. All MRI examinations consistently increased each year except those done of the extremities. The indications for MRI were acute neurologic/behavioral problem and trauma. Computed tomography of the head, abdomen, and cervical spine and MRI of the head, neck, and lumbar spine are the vast majority of ED-ordered studies at this institution as well as others reported in the literature [2,3]. The role of MRI has expanded in the evaluation of patients with transient ischemic attacks and minor strokes to become the preferred imaging modality [10,26]. Magnetic resonance imaging and MRA can be used to evaluate for subarachnoid hemorrhage, aneurysm, venous thrombosis, and vasculitis [26]. This may explain why MRI/MRA of the head increased each year and may have replaced head CT for select patient populations.
The last focus of our study was on the relationship between CT and MRI for individual patients. Of patients who had MRI done in our ED, 89.4% also had a CT done within 3 calendar days. Most of these occurred during the ED visit. Of this group, 45.7% had the MRI done of the same anatomical area as the CT with brain imaging in the overwhelming majority of studies. This might be explained by either a significant abnormality on the head CT or by High clinical suspicion in the presence of a nondiagnostic head CT.
In summary, there was a steady increase in MRI testing in our academic ED between 2007 and 2011. Most of these were done of the head for acute neurologic or behavioral changes. There was a corresponding decreasing trend for CT scans. The decline was noticeable for abdominal CT scans, which were primarily ordered for trauma and/or abdominal pain; 45.7% of patients who had an MRI ordered in the ED had a CT done of the same anatomical location within 3 days, and again, most of these were head/brain.
The authors would like to thank Teri Defor for her assistance with data abstraction and data table creation.
References
- Agarwal R, Bergey M, Sonnad S, et al. Inpatient CT and MRI utilization: trends in the Academic hospital setting. J Am Coll Radiol 2010;7:949-55.
- Rao V, Levin D, Parker L, et al. Trends in utilization rates of the various imaging modalities in emergency departments: nationwide Medicare data from 2000 to 2008. J Am Coll Radiol 2011;8(10):706-9.
- Lee J, Kirschner J, Pawa S, et al. Computed tomography use in the adult emergency department of an academic urban hospital from 2001-2007. Ann Emerg Med 2010;56:591-6.
- Larson D, Johnson L, Schnell BM, et al. National trends in CT use in the emergency department: 1995-2007. Radiology 2011;258(1):164-73.
- Kocher KE, Meurer WJ, Fazel R, et al. National trends in use of computed tomography in the emergency department. Ann Emerg Med 2011;58:452-62.
- Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007;357:2277-84.
- Miglioretti DL, Johnson E, Williams A, et al. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 2013;167(8):700-7.
- Sodickson A, Baeyens PF, Andriole KP, et al. Recurrent CT, cumulative radiation exposure and associated radiation-induced cancer risks from CT of adults. Radiology 2009;251:175-84.
- Gerischer LM, Fiebach JB, Scheitz JF, et al. Magnetic resonance imaging-based versus computed tomography-based thrombolysis in acute ischemic stroke: comparison of safety and efficacy within a cohort study. Cerebrovasc Dis 2013;35(3): 250-6.
- Forster A, Gass A, Kern R, et al. Brain imaging in patients with transient ischemic attack: a comparison of computed tomography and magnetic resonance imaging. Eur Neurol 2012;67(3):136-41.
- Revel MP, Sanchez O, Couchon S, et al. Diagnostic accuracy of magnetic resonance imaging for an acute pulmonary embolism: results of the “IRM-EP” study. J Thromb Haemost 2012;10(5):743-50.
- Larsson EM, Holtas S, Crongvist S, et al. Comparison of myelography, CT myelography and magnetic resonance imaging in cervical spondylosis and disk herniation. Pre- and postoperative findings. Acta Radiol 1989;30(3):233-9.
- Cobben L, Groot I, Kingma L, et al. A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol 2009;19(5):1175-83.
- Lipinski MJ, McVey CM, Berger JS, et al. Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 2013;62(9):826-38.
- Leurent G, Langella B, Fougerou C, et al. diagnostic contributions of cardiac magnetic resonance imaging in patients presenting with elevated troponin, acute chest pain syndrome and unobstructed coronary arteries. Arch Cardiovasc Dis 2011;104(3):161-70.
- Akhtar JI, Spear RM, Senac MO, et al. Detection of traumatic brain injury with magnetic resonance imaging and S-100B protein in children, despite normal computed tomography of the brain. Pediatr Crit Care Med 2003;4(3):322-6.
- Rankey D, Leach JL, Leach SD. Emergency MRI utilization trends at a tertiary care academic medical center: baseline data. Acad Radiol 2008;15:438-43.
- Raja AS, Andruchow J, Zane R, et al. Use of neuroimaging in US emergency departments. Arch Int Med 2011;171:260-2.
- Smulowitz PB, Ngo L, Epstein SK. The effect of a CT and MR preauthorization program on ED utilization. Am J Emerg Med 2009;27:328-32.
- Boulanger BR, Kearney PA, Brenneman FD, et al. Utilization of FAST (Focused Assessment with Sonography for Trauma) in 1999: results of a survey of North American trauma centers. Am Surg 2000;66:1049-55.
- Sheng AY, Daiziel P, Liteplo AS, et al. Focused assessment with sonography in trauma and Abdominal computed tomography utilization in adult trauma patients: trends over the last decade. Emerg Med Int 2013:678380.
- Babcock D. Sonography of the acute abdomen in the pediatric patient. J Ultrasound
Menoch MJA, Hirsh DA, Khan NS, et al. Trends in computed tomography utilization in the pediatric emergency department. Pediatrics 2012;129:e690-7.
- Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 2005;58(5):902-5.
- Como J, Diaz J, Dunham CM, et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the Eastern Association for the Surgery of Trauma Practice Management Guidelines Committee. J Trauma 2009;67:651-9.
- Moreau F, Asdaghi N, Modi J, et al. Magnetic resonance imaging versus computed tomography in transient ischemic attack and minor stroke: the more you see the more you know. Cerebrovasc Dis Extra 2013;3:130-6.
