Late presentation of blunt right diaphragmatic rupture (hepatic hernia)
Case Report
Late presentation of blunt right diaphragmatic rupture (hepatic hernia)
Abstract
Diaphragmatic rupture occurs in 0.8% to 3.6% of patients after blunt or penetrating thoracoabdominal trauma, and the preoperative diagnosis is difficult. The diagnosis of traumatic diaphragmatic rupture may be made on initial presentation or at any time later. Right-sided diaphragmatic rupture is rare and occurs in approximately 5% to 20% of all diaphragmatic disruptions. The incidence of herniation of the intra-abdominal organs into the Pleural cavity is also low, observed in only about 19% of right-sided diaphrag- matic ruptures. We present a case of right-sided traumatic rupture of the diaphragm diagnosed 15 years after the initial blunt trauma. A 22-year-old male patient fell 15 years before and was symptom-free since then. He was referred to our hospital with the signs of herniation of the right diaphragm, which was manifested in the chest X-rays. The definite diagnosis was made through thoracoAbdominal computed tomography. The diaphragmatic rupture was repaired via abdominal approach.
Diaphragmatic rupture (DR) occurs in 0.8% to 3.6% of patients after blunt thoracoabdominal trauma, and the preoperative diagnosis is difficult. The diagnosis of traumatic DR could be made on initial presentation or at any time later. Diaphragmatic rupture on the left side occurs in 90% of the cases. Whereas a plain chest x-ray film suggests the diagnosis in only 17% to 40% of patients, computed tomography (CT) scan could be a helpful addition in the investigation [1]. We present a case with right-sided DR and herniation of the liver, gall bladder, proximal transverse, and distal Ascending colon, which was diagnosed 15 years after the initial blunt trauma.
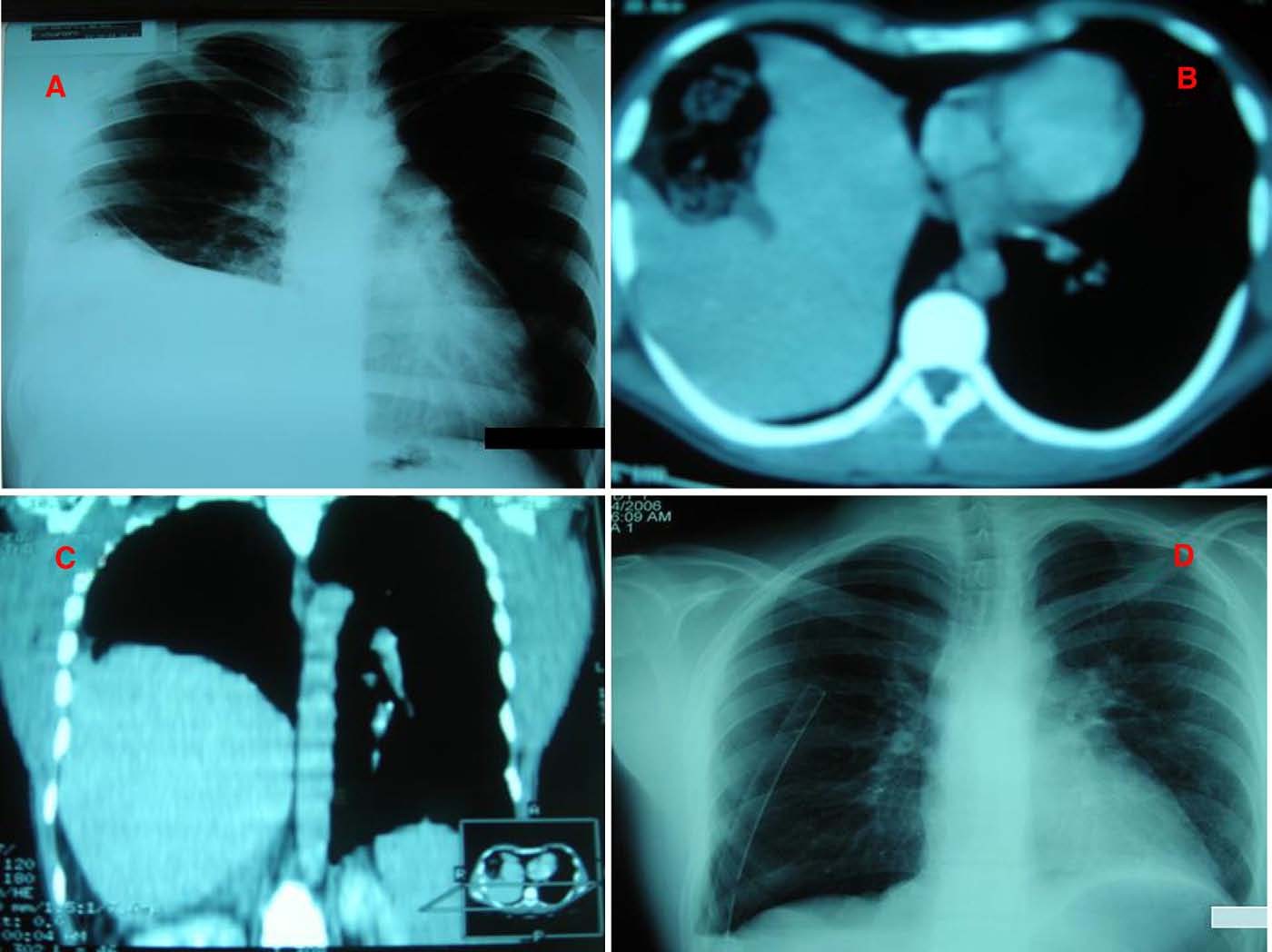
A 22-year-old man who was having cough for 1 week was admitted to our hospital emergency department. Fifteen years before, he fell at a height of nearly 4 m, but he had no complications. On his physical examination, bowel sounds were audible in the right lower thorax, and the diaphragm was determined to be higher of the right side by percussion. Chest x-rays showed a high right diaphragm (Fig. 1A). Thoracoab- dominal CT demonstrated right-sided DR with intrathoracic
protrusion of the right hepatic lobe, gallbladder, proximal transverse and distal ascending colon (Fig. 1B, C). Elective surgery was carried out through a midline laparotomy. The size of the defect was 10 x 15 cm, and the gap was through the right hemithorax (Fig. 2). The hernia contained the gallbladder and large intestine. The defect was repaired with nonabsorbable running sutures. Postoperative course was uneventful, and chest radiographs showed a normally aerated right lower lobe (Fig. 1D). The patient was discharged from the hospital on the sixth postoperative day.
Traumatic DR is an uncommon but severe problem in a patient with multiple injuries. Blunt or penetrating thor- acoabdominal traumas can result in DR. The reported incidence of DR is between 0.8% and 3.6% of patients admitted to the emergency unit with blunt thoracoabdominal trauma [2-4]. Traffic accidents and high falls are mostly responsible of diaphragmatic Blunt injuries. Right-sided DR is rare and occurs in approximately 5% to 20% of all diaphragmatic disruptions. The incidence of herniation of the intra-abdominal organs into the pleural cavity is low and observed in only about 19% of right-sided DRs. (It is observed in 58% of left-sided DRs [1,5,6].) The preoperative diagnosis of traumatic DR is difficult. Patients with undiagnosed rupture of the diaphragm can develop symp- toms after a delay of weeks, months, or even years. The diagnosis of the diaphragmatic hernia may be possible in only 25% to 50% of the cases after the trauma [7]. Abdominal and lower thorax pain, dyspnea, cyanosis, cardiac arrhythmia, and hypotension are Typical symptoms of DR, or the patient, like ours, may be completely asymptomatic. Diaphragmatic rupture is usually diagnosed during exploration for other injuries. A high index of suspicion is required to diagnose blunt DR.
Abnormalities are shown on the chest x-ray obtained at the time of injury, but X-ray findings are suggestive of the diagnosis in only 17% to 40% of patients [1,2,8]. In this case, the right diaphragm was elevated on the chest x-ray. The use of sonography in the diagnosis of DR has been reported, but it is dependent on the operator’s skill and often limited in the setting of acute trauma. A CTscan can be a helpful addition in the investigation, allowing pulmonary contusions and hemothoraces to be diagnosed and distinguished from DR with herniation of visceral organs (ie, hepatic lobe, gall bladder, large and Small intestines) into the pleural cavity. Helical CT has an average sensitivity and specificity of 61%
0735-6757/$ – see front matter (C) 2008
 638.e4 Case Report
638.e4 Case Report
Fig. 1 A, Preoperative chest x-ray showing the right diaphragm revealed higher localization. B and C, Axial and coronal CT scan of the thorax revealed intrathoracic displacement of the liver. D, Postoperative chest x-ray: the limits of the right hemidiaphragm are well defined.
and 87%, respectively [9]. In our case, signs of DR consisting of a constricting rim around the herniated right and left hepatic lobe caused by the torn diaphragm were on the CT. Scintigraphy of the liver by 99mTc is also beneficial in diagnosis of a suspicious case. Magnetic resonance presents a high sensitivity of the diaphragmatic outline and shows DR and intrathoracic herniation. However, this technique cannot be performed in emergency situations or in multitrauma patients [2,10,11].
Diaphragmatic rupture may fall into 2 categories; type I, those patients with immediate or early symptoms after the trauma (early), and type II, delayed (as in our patient). The diagnosis and the treatment of DR and hernia may be achieved during immediate operation or years (15 years as with our patient) later. An increased morbidity and mortality are related to a delayed diagnosis of traumatic DR. However, the mortality associated with right-sided DR within the first 24 hours is reported to be 31% [1,5,7]. Therefore, the diagnosis should be kept in mind in abdominal trauma with blunt thoracic injury, pelvic fracture, and hypoxemia [7].
The surgical treatment of DR should be performed through an abdominal route. The abdominal organs are replaced into the abdominal cavity. The diaphragmatic defect
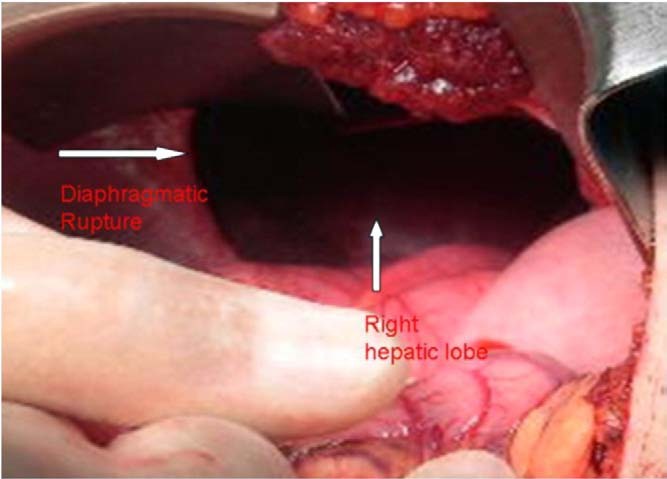
Fig. 2 Intraoperative view of DR.
is sutured by unabsorbable material, placed interruptedly, and when possible, a 2-layer closure should be performed. Synthetic grafts are generally not required. Some authors favor a thoracotomy to repair a right-sided DR. However, abdominal route ensures identification of any associated abdominal injuries, which occurs in 30% to 70% of patients. Thoracotomy is performed when there are thoracic injuries, large herniation, and empyema are developed. In delayed cases, this procedure may be recommended [1,2,5,12]. Our patient was a delayed case that had a chest x-ray and a thoracoabdominal CT scan. A right diaphragm raise was shown, and the suspected DR with dislocation of the liver and other organs was confirmed. In this case, the abdominal repair was successful.
In conclusion, after blunt trauma, to diagnose DRs, a high index of suspicion need not exist. In Delayed presentations, questioning for a trauma history is essential.
Orhan Kozak MD Oner Mentes MD Ali Harlak MD Taner Yigit MD Zafer Kilbas MD Ismail Aslan MD
Department of General Surgery Gulhane Military Medical Academy
Ankara, Turkey
Murat Akin MD Department of General Surgery Gulhane Military Medical Academy
Ankara, Turkey Department of General Surgery Gazi University of Medical School
Ankara, Turkey Email-address: [email protected]
Ugur Bozlar MD
Department of Radiology Gulhane Military Medical Academy
Ankara, Turkey
doi:10.1016/j.ajem.2007.10.032
References
- Wirbel RJ, Mutschler W. Blunt rupture of the right hemi-diaphragm with complete dislocation of the right hepatic lobe: report of a case. Surg Today 1998;8:850-2.
- Sacco R, Quitadamo S, Rotolo N, et al. Traumatic diaphragmatic rupture: personal experience. Acta Biomed 2003;74:71-3.
- Mihos P, Potaris K, Gakidis J, et al. Traumatic rupture of the diaphragm: experience with 65 patients. Injury 2003;3:169-72.
- Reber PU, Schmied B, Seiler CA, et al. Missed diaphragmatic injuries and their long-term sequelae. J Trauma 1998;44:183-8.
- Boulanger BR, Milzman DP, Rosati C, et al. A comparison of right and left blunt traumatic diaphragmatic rupture. J Trauma 1993;35: 255-60.
- Tribble JB, Julinan S, Myers RT. Rupture of the liver and right hemi- diaphragm presenting as right hemothorax. J Trauma 1989;29:116-8.
- Peker Y, Tatar F, Kahya MC, et al. Dislocation of three segments of the liver due to hernia of the right diaphragm. Report of a case and review of the literature. Hernia 2007;11:63-5.
- Gelman R, Mirvis SE, Gens D. Diaphragmatic rupture due to blunt trauma. Sensitivity of plain chest radiographs. AJR Am J Roentgenol 1991;156:51-7.
- Sadeghi N, Nicaise N, DeBacker D, et al. Right diaphragmatic rupture and hepatic hernia: an indirect sign on computed tomography. Eur Radiol 1999;9:972-4.
- Hoang AD, De Backer D, Bouazza F, et al. Undiagnosed rupture of right hemi diaphragm-hepatothorax: a case report. Acta Chir Belg 2002;5:353-65.
- Shanmuganathan K, Mirvis SE, White CS, Pomerantz SM. MR imaging evaluation of hemi diaphragms in acute blunt trauma: experience with 16 patients. AJR Am J Roentgenol 1996;167:397-402.
- Liu DW, Liu HP, Lin PJ, et al. Video-assisted thoracic surgery in treatment of chest trauma. J Trauma 1997;42:670.
