Impact of computerized physician order entry on ED patient length of stay
Brief Report
Impact of computerized physician Order entry on ED patient length of stay?,??
Shaun C. Spalding MD a, Paula H. Mayer MD b, Adit A. Ginde MD, MPH b,
Steven R. Lowenstein MD, MPH b, Michael Yaron MD b,?
aDenver Health and Hospitals, Residency in Emergency Medicine, Denver, CO 80204, USA bDivision of Emergency Medicine and the Colorado Emergency Medicine Research Center, University of Colorado Denver School of Medicine, Aurora, CO 80045, USA
Received 22 June 2009; revised 29 September 2009; accepted 20 October 2009
Abstract
Objectives: We evaluated whether implementation of Computerized physician order entry reduces length of stay (LOS) for discharged emergency department (ED) patients.
Methods: Emergency department LOS for discharged and admitted patients were analyzed in a university- affiliated ED before and after introduction of CPOE. Patient demographics and covariates that may affect LOS (mode of arrival, provider staffing, Daily census, and admission rate) were measured.
Results: The study included 71 188 patients; 49 175 (69%) were discharged from the ED (28 687 before and 20 488 after CPOE). Length of stay for discharged patients decreased from 198 to 168 minutes (difference of -30; 95% confidence interval [CI], -28 to -33), whereas LOS for admitted patients increased from 405 to 441 minutes (difference of +36; 95% CI, 26-46). After controlling for covariates, CPOE implementation was associated with a 23-minute decrease in LOS for discharged patients (? = -23 [95% CI, -26 to -19]).
Conclusion: Implementation of CPOE was associated with a clinically significant (23-minute) decrease in LOS among patients who were discharged from the ED.
(C) 2011
Introduction
Emergency department (ED) length of stay (LOS) is an important measure of practice efficiency and a critical determinant of patient satisfaction [1]. Long patient LOS are
? Abstract presented at the 2008 American College of Emergency Physicians Research Forum, Chicago, Ill, October 27, 2008.
?? This study was supported in part by a grant from Picis, Inc,
Wakefield, Mass.
* Corresponding author. Tel.: +1 720 848 6777.
E-mail address: [email protected] (M. Yaron).
also associated with lost revenues for hospitals, due to Ambulance diversions and larger numbers of patients who leave without being seen or before treatment is completed [2-5]. Many factors contribute to ED LOS, including high patient volumes and a lack of inpatient beds [6-13]. The result of these factors is ED crowding, which strains limited resources, adversely affects patient outcomes, and over- whelms the capacity of many EDs [10,14-19].
Several studies have evaluated interventions that seek to decrease ED LOS. Fast-track pathways, urgent care areas [20,21], ED expansion [22], in-room registration [23], short- stay Observation Units (eg, for patients with chest pain or asthma) [24], on-site laboratory test processing [25,26], and
0735-6757/$ - see front matter (C) 2011 doi:10.1016/j.ajem.2009.10.007
triage kiosks in ED waiting rooms [27] have shown promise in reducing LOS. Simultaneous application of several interven- tions may have an additive, favorable effect on LOS [16].
computerized physician order entry has been associated with improvED efficiency and decreased LOS in critical care settings [28-31]. In the ED, CPOE has been reported to reduce the time that nurses spend in clarifying and responding to medication, laboratory, and radiology orders [32]. In a small study of patients with stroke symptoms, Nam et al [33] reported that CPOE was associated with a significant reduction in time from patient arrival to thrombolysis. The reduction stemmed from faster turnaround of laboratory and diagnostic Imaging results and more rapid completion of orders.
To our knowledge, no study has evaluated the association between CPOE and ED LOS. The objective of this study was to measure the effect of CPOE implementation on the LOS of patients discharged from the ED.
Methods
Study design
A before-and-after study design was used to compare ED patient LOS while using a paper-based, written order entry system to the LOS after implementation of CPOE. The Colorado Multiple Institution Review Board approved this investigation.
Study setting and participants
The study was conducted at an urban, academic, hospital- affiliated ED. The hospital is a level 2 trauma center, and the ED census is approximately 35 000 ED visits per year. Throughout the study period, an emergency department information system (EDIS; Picis PulseCheck, Waltham, Mass) was used for patient tracking, laboratory result reporting, and electronic chart documentation by both physicians and nurses. Our study period began in March 1, 2005, 1 month after completion of our initial EDIS installation. Fifteen months later, CPOE was implemented in June 2007. After CPOE implementation, data collection continued for 12 additional months, ending on May 31, 2008, 3 weeks before the hospital closed and moved to a new facility. Thus, patient LOS was compared during 2 time periods: 15 months before CPOE and 12 months after CPOE. All patients triaged to, and discharged from, the ED during the study period were included in the data analysis. Patients who Left without being seen or who were triaged to other hospital areas (eg, the obstetrics labor ward) were excluded from analysis. Although we were primarily interested in ED LOS for discharged patients, patient LOS was also calculated for ED patients admitted to the hospital
as a measure of crowding and ED bed availability.
Interventions
Before CPOE introduction, all orders for laboratory tests, radiology studies, and medications were handwritten and recorded on standardized paper forms. Order forms were stored in a binder (the patient’s ED chart), which was housed at the nursing station closest to the patient’s room. Color- coded tags on the charts were used to signal that a new order was ready for clerk and nurse processing.
Radiology and pharmacy orders had to be faxed to the appropriate department to initiate processing. Laboratory orders required the nurse to obtain identification stickers from the ED clerk, apply them to test samples, and send them to the laboratory with completed laboratory paperwork. Laboratory personnel transcribed the written order informa- tion into their computer system and generated new bar-coded labels that were affixed to the test samples. Then, automated processing of the samples began. Results were available electronically when completed.
Radiology studies were processed electronically and posted to the Picture Archiving and Communication System. Before CPOE, physicians needed to open the Picture Archiving and Communication System software to deter- mine whether a study was completed and ready for viewing. Interpretations by radiologists were faxed to the ED, and urgent readings were communicated by telephone.
The CPOE system enabled physicians and nursing staff to order laboratory tests, diagnostic imaging studies, nursing procedures, and patient medications. Electronic order sets were created to allow clinicians to easily locate specific tests, medications, and procedures from electronic menus. Orders were sent electronically to the appropriate site (laboratory, radiology, and nursing). Computer interfaces between the ED and laboratory computers enabled immediate printing of bar-coded patient identification stickers at the appropriate ED nursing station. Tests were labeled by the nurse and sent to the laboratory, where automated test processing began immediately. Clerical staff members no longer processed orders. Once orders were completed, results were transmitted electronically to the EDIS, and clinicians received an electronic notice that test results were ready for viewing.
During CPOE implementation, a 30-minute instructional session was provided to all permanent staff members. Subsequently, on a monthly basis, new rotating house staff received a 1.5-hour training session on use of the EDIS, including CPOE. These monthly training sessions were conducted by the same attending physician throughout the study period.
Measurements
All ED triage and patient care times were recorded electronically in an identical manner by the EDIS before and after implementation of CPOE. Patient LOS was defined as the time from triage to discharge from the ED.
The time of discharge was recorded when the patient physically left the ED and the patient was removed from the electronic tracking screen. Patient demographics (age, sex, and race) and other covariates that were likely to affect LOS were measured, including mode of patient arrival (ambulance or nonambulance), physician and nurse staffing hours, daily ED census, and daily admission rate. physician staffing hours were collected from staffing schedules during the study time periods. The daily number of hours worked by attending physicians, resident physicians, and intern physicians were recorded.
Data analysis
Demographic and clinical characteristics of patients and mean daily LOS data were compared before and after implementation of CPOE. Student t test was used to compare means for measurement variables; categorical data were compared using the ?2 test.
Multivariable linear regression analysis was used to test for an association between CPOE implementation and LOS, after adjusting for the effects of physician and nursing staffing, daily ED census, admission rate, mode of arrival, and patient demographics.
Results
During the 27-month study period, 71 188 patients were cared for in the ED; of these, 49 175 were discharged from the ED and were included in the primary data analysis. There were 28 687 patients discharged before and 20 488 patients discharged after CPOE implementation. No clinically
Table 1 Patient demographics and clinical covariates before and after implementation of CPOE a
|
No. patients discharged 28 687 20 488
Age (y) +- SEM 37.7 +- 0.10 38.5 +- 0.12 Daily census (patients +- SEM) 83 +- 0.060 78 +- 0.074 Sex (% male) 45 45 Race (%) White 54 56 Black 18 18 Hispanic 22 20 Other 6 6 Arrival by ambulance (%) 7.3 9.5 Admission rate (%) 21 20.2 Staffing Attending (h/d) +- SEM 36 +- 0 35.8 +- 0.004 Resident (h/d) +- SEM 51 +- 0.02 45 +- 0 Intern (h/mo) +- SEM 1372 +- 0.96 1392 +- 2.53 |
|
a Due to the large sample size, all differences, except for sex, were statistically significant (P b .001). |
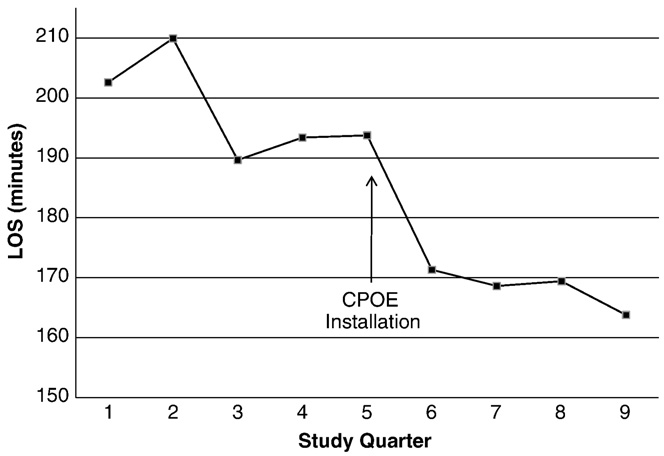
Fig. 1 Length of stay for discharged patients (by quarter), before and after CPOE.
significant differences in age, sex, race, or daily admission rate before and after CPOE implementation were found. The daily census decreased from 83 to 78 patients per day (difference -5.2; 95% confidence interval [CI], -5.0 to -5.3) after CPOE implementation. The percentage of ambulance arrivals increased from 7.3% to 9.5% (difference +2.2%;
95% CI, 1.7%-2.7%; Table 1).
No computer downtimes occurred before or after CPOE implementation. A brief planned downtime (b1 hour) occurred on the day of CPOE implementation.
Emergency department LOS for patients discharged from the ED decreased from 198 to 168 minutes (difference -30 minutes; 95% CI, -28 to -33; Fig. 1). In contrast, LOS for admitted patients increased from 405 to 441 minutes (difference +36 minutes; 95% CI, 26-46). After controlling for daily census and demographic and clinical covariates, CPOE implementation maintained an independent inverse association with LOS for discharged patients (? = -23; 95% CI, -26 to -19).
Discussion
In the present study, implementation of a CPOE system to our existing EDIS resulted in an overall reduction of ED LOS for discharged patients by 23 minutes, after adjusting for patient demographics, ED census, mode of arrival, Hospital admission rate, and provider staffing. The reduction occurred despite an increase in overall crowding, as measured by the LOS for patients admitted to the hospital. We assume that the increased time of boarded patients in the ED resulted in fewer examination rooms and thus reduced the ED bed availability for potentially dischargeable patients. With fewer “open” beds available for patient care, the LOS still decreased for discharged patients after implementing CPOE. The reasons for this effect may be multifactorial. The CPOE system computer interface enables data transfer and communication of orders on a real-time basis without the
need for further staff intervention. It is likely that ordering and reporting of laboratory and diagnostic studies becomes more efficient with electronic processing. Improved report- ing efficiency allows for more timely reactions to and implementation of Treatment regimens and protocols. Paper- based order entry required extra steps of communication and data entry beyond the written orders. The time required for our staff to recognize and send new orders from our ED, along with additional processing time in the laboratory or radiology departments, may have delayed order entry and increased the time to results reporting.
Examination of the first 2 months after CPOE installa- tion showed no increase in LOS. Thus, the data did not suggest any adverse effect from the transition to the new CPOE system.
Many studies have evaluated other interventions in the ED to decrease LOS. Reported reductions in ED LOS range from 10 to 15 minutes with implementation of a Rapid admission policy and in-room registration to as much as 1.8 hours with use of a short-stay observation unit in the ED [3,23-26,34]. Our results of a 23-minute decrease in ED LOS fall within the range of ED LOS reductions from other modalities in other studies. The main difference is that we evaluated ED LOS for discharged patients, whereas most other studies have only evaluated LOS for all patients in the ED. Further investigation is needed to know if simultaneous application of these interventions could have an additive effect on LOS.
Limitations
Our assessment of the impact of CPOE implementation in our ED has several potential limitations. The most important is that this study was conducted in a single urban teaching ED, with relatively long baseline lengths of stay for treat- and-release patents. In other ED settings, with different patient acuities, Hospital resources and ED staffing and workflow patterns, the results might be different.
Our administrative data set did not include accurate information regarding nurse staffing hours. In addition, there are other unmeasured covariates that are likely to affect patient LOS. patient acuity, comorbidity, seasonal factors, triage and clinical care protocols, laboratory and radiology processing times, and use of specialty consultations were not measured in this study; yet, any of these factors could have influenced LOS, independent of the implementation of CPOE. We could not measure these system-, provider-, and patient-related variables, although we have no reason to suspect that they changed materially after CPOE implemen- tation. In addition, there were no changes to the waiting room or patient care areas during the study period.
The average daily census was lower in the post-CPOE period, which could have confounded the relationship between CPOE implementation and LOS. However, we
controlled for daily census in the multivariate model. We also found that despite the lower daily census, the LOS for admitted patients still increased. We suspected that the increase in LOS for admitted patients was a measure of hospital and ED crowding. If true, then the decline in LOS for discharged patients that we observed becomes even more important. We acknowledge that LOS for admitted ED patients is not a validated measure of ED crowding. A validated measure, such as the Emergency Department Work Index score, may provide a better measure of crowding and should be considered for future prospective studies [35].
Finally, patient LOS was the only “outcome” variable we measured in this study. We did not measure changes in the quality of care, error rates, patient satisfaction, or resource utilization after implementation of CPOE.
Conclusions
In this academic ED, implementation of a CPOE system was associated with a clinically significant (23-minute) decrease in LOS among patients who were discharged from the ED, despite evidence of longer Boarding times for admitted patients. Replacing paper-based written and verbal orders with more efficient computerized orders and real-time reporting of test results may explain this favorable effect. Interventions that decrease LOS may improve patient satisfaction, reduce the number of patients who are leaving without being seen, decrease the frequency of ambulance diversions, trim the time from patient presentation to treatment, and improve health care outcomes.
References
- Cassidy-Smith TN, Baumann BM, Boudreaux ED. The disconfirma- tion paradigm: throughput times and emergency department patient satisfaction. J Emerg Med 2007;32:7-13.
- Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med 2008 [Epub].
- Falvo T, Grove L, Stachura R, et al. The opportunity loss of boarding admitted patients in the emergency department. Acad Emerg Med 2007;14(4):332-7.
- Falvo T, Grove L, Stachura R, et al. The Financial impact of ambulance diversions and patient elopements. Acad Emerg Med 2007;14:58-62.
- Boudreaux ED, Friedman J, Chansky ME, et al. Emergency department patient satisfaction: examining the role of acuity. Acad Emerg Med 2004;11(2):162-8.
- Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data 2007: 1-32.
- Committee On Pediatric Emergency Medicine. Overcrowding crisis in our nation’s emergency departments: is our safety net unraveling? Pediatrics 2004;114:878-88.
- Timm NL, Ho ML, Luria JW. Pediatric emergency department overcrowding and impact on patient flow outcomes. Acad Emerg Med 2008;15(9):832-7.
- Forster AJ, Stiell I, Wells G, et al. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med 2003;10(2):127-33.
- Olshaker JS, Rathlev NK. Emergency Department overcrowding and ambulance diversion: the impact and potential solutions of extendED boarding of admitted patients in the emergency department. J Emerg Med 2006;30(3):351-6.
- Rathlev NK, Chessare J, Olshaker J, et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med 2007;49(3):265-71.
- Chan L, Reilly KM, Salluzzo RF. Variables that affect Patient throughput times in an academic emergency department. Am J Med Qual 1997;12(4):183-6.
- Yoon P, Steiner I, Reinhardt G. Analysis of factors influencing length of stay in the emergency department. CJEM 2003;5:155-61.
- Aldeen AZ, Gisondi MA. Bedside teaching in the emergency department. Acad Emerg Med 2006;13(8):860-6.
- Colpaert K, Claus B, Somers A, et al. Impact of computerized physician order entry on Medication prescription errors in the intensive care unit: a controlled cross-sectional trial. Crit Care 2006;10:R21.
- Twanmoh JR, Cunningham GP. When overcrowding paralyzes an emergency department. Manag Care 2006;15(6):54-9.
- Shulman R, Singer M, Goldstone J, et al. Medication errors: a prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care 2005;9(5):R516-R521.
- Kuperman GJ, Teich JM, Gandhi TK, et al. Patient safety and computerized medication ordering at Brigham and Women’s Hospital. Jt Comm J Qual Improv 2001;27(10):509-21.
- Jayawardena S, Eisdorfer J, Indulkar S, et al. Prescription errors and the impact of computerized prescription order entry system in a community-based hospital. Am J Ther 2007;14(4):336-40.
- Darrab AA, Fan J, Fernandes CM, et al. How does fast track affect quality of care in the emergency department? Eur J Emerg Med 2006;13(1):32-5.
- O’Brien D, Williams A, Blondell K, et al. Impact of streaming “fast track”
emergency department patients. Aust Health Rev 2006;30(4):525-32.
- Han JH, Zhou C, France DJ, et al. The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med 2007;14(4):338-43.
- Gorelick MH, Yen K, Yun HJ. The effect of in-room registration on emergency department length of stay. Ann Emerg Med 2005;45: 128-33.
- Bazarian JJ, Schneider SM, Newman VJ, et al. Do admitted patients held in the emergency department impact the throughput of treat-and- release patients? Acad Emerg Med 1996;3:1113-8.
- Singer AJ, Viccellio P, Thode Jr HC, et al. Introduction of a Stat laboratory reduces emergency department length of stay. Acad Emerg Med 2008;15(4):324-8.
- Holland LL, Smith LL, Blick KE. Reducing laboratory turnaround time outliers can reduce emergency department patient length of stay: an 11-hospital study. Am J Clin Pathol 2005;124(5):672-4.
- Sign-in kiosks shorten waiting room lines. ED Manag 2007;19(12): 137-8.
- Ali NA, Mekhjian HS, Kuehn PL, et al. Specificity of computerized physician order entry has a significant effect on the efficiency of workflow for critically ill patients. Crit Care Med 2005;33(1):110-4.
- Kuperman GJ, Gibson RF. computer physician order entry: benefits, costs, and issues. Ann Int Med 2003;139:31-9.
- Chertow GM, Lee J, Kuperman GJ, et al. Guided medication dosing for inpatients with renal insufficiency. J Am Med Assoc 2001;286: 2839-44.
- Mekhjian HS, Kumar RR, Kuehn L, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center. J Am Med Inform Assoc 2002;9:529-39.
- Banet GA, Jeffe DB, Williams JA, et al. Effects of implementing computerized practitioner order entry and nursing documentation on nursing workflow in an emergency department. J Healthc Inf Manag 2006;20(2):45-54.
- Nam HS, Han SW, Ahn SH, et al. Improved time intervals by implementation of computerized physician order entry-based stroke team approach. Cerebrovasc Dis 2007;23(4):289-93.
- Quinn JV, Mahadevan SV, Eggers G, et al. Effects of implementing a rapid admission policy in the ED. Am J Emerg Med 2007;25(5): 559-63.
- Bernstein SL, Verghese V, Leung W, et al. Development and validation of a new index to measure emergency department crowding. Acad Emerg Med 2003;10(9):938-42.