Median arcuate ligament syndrome presenting as hemorrhagic shock
American Journal of Emergency Medicine 31 (2013) 1152.e1-1152.e4
Contents lists available at SciVerse ScienceDirect
American Journal of Emergency Medicine
journal homepage: locate/ ajem
Case Report
Median arcuate ligament syndrome presenting as hemorrhagic shock
 Abstract
Abstract
The major symptoms of median arcuate ligament syndrome, celiac axis stenosis, or occlusion compressed by the median arcuate ligament include eating-associated abdominal pain and weight loss. Because celiac stenosis increases retrograde collateral blood flow from the Superior mesenteric artery to the Celiac artery via the pan- creaticoduodenal arcade, a pancreaticoduodenal artery aneurysm could occur at a low incidence rate. Rupture of the pan- creaticoduodenal artery aneurysm and hemorrhagic shock are rare. In this report, we present 3 cases of patients who had been well with no abdominal symptoms until the day of admission, when they experienced sudden-onset intra-Abdominal hemorrhage and shock. These 3 patients were admitted to the emergency department, and contrast-enhanced computed tomography and radiographic selective catheter angiography revealed intra-abdominal hemorrhage, stenosis of the celiac arteries, and dilated pancreaticoduodenal arcade. Case 1 demonstrated severe hemorrhagic shock, whereas case 2 demon- strated moderate shock. We treated ruptured pancreaticoduodenal artery aneurysms with coil embolization. Case 3 demonstrated complete celiac occlusion and moderate hemorrhagic shock, and no aneurysm was detected.
Median arcuate ligament syndrome, celiac axis stenosis, or occlusion compressed by the median arcuate ligament rarely cause upper abdominal pain [1,2]. The celiac stenosis increases retrograde collateral blood flow from the superior mesenteric artery (SMA) to the celiac artery perfusion area via pancreaticoduodenal arcade and could form pancreaticoduodenal artery aneurysms. We describe 3 patients who presented to the emergency department of the hospital with sudden-onset intra-abdominal hemorrhage and shock.
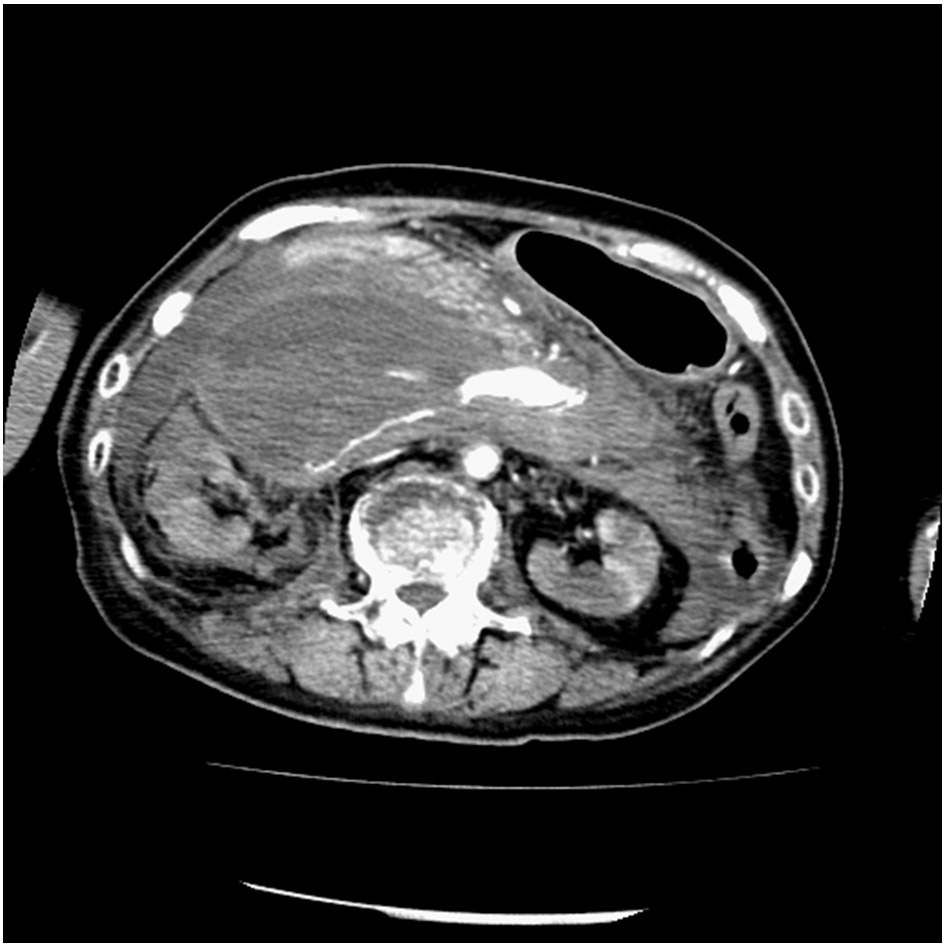
A 69-year-old woman was transferred to the emergency depart- ment of the hospital because of sudden collapse and hypotension. She had a history of atrial fibrillation and was currently taking warfarin. She was healthy and without any abdominal symptoms or trauma history until the day of admission. Upon admission, her blood pressure was 52/immeasurable mm Hg; pulse rate, 130 beats/min; respiratory rate, 36 breaths/min; hemoglobin level, 5.2 g/dL; and hematocrit, 15.9%. Abdominal contrast-enhanced computed tomog- raphy (CT) revealed a massive Retroperitoneal hematoma around the head of the pancreas with active Arterial extravasation and focal narrowing of the celiac axis (Fig. 1 and 2). Radiographic selective catheter angiography of the SMA revealed retrograde blood flow from the SMA to the celiac artery via the pancreaticoduodenal arcade and extravasations from the inferior pancreaticoduodenal artery and posterior superior pancreaticoduodenal artery (Fig. 3). The extrava- sations were effectively treated with transcatheter arterial emboliza- tion (TAE) using platinum coils.
Fig. 1. Massive hematoma with arterial extravasation shown on contrast-enhanced CT.
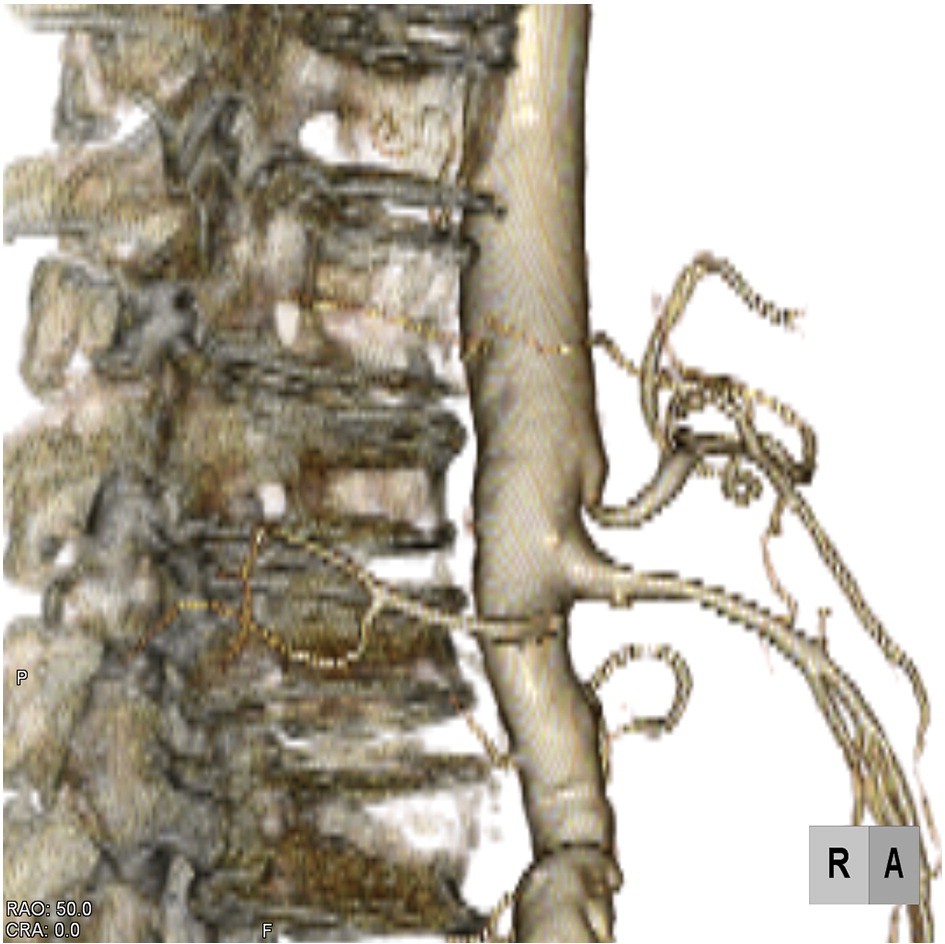
Fig. 2. Celiac axis stenosis shown on 3-dimensional CT angiography.
0735-6757/$ - see front matter (C) 2013
1152.e2 Y. Matsumura et al. / American Journal of Emergency Medicine 31 (2013) 1152.e1-1152.e4
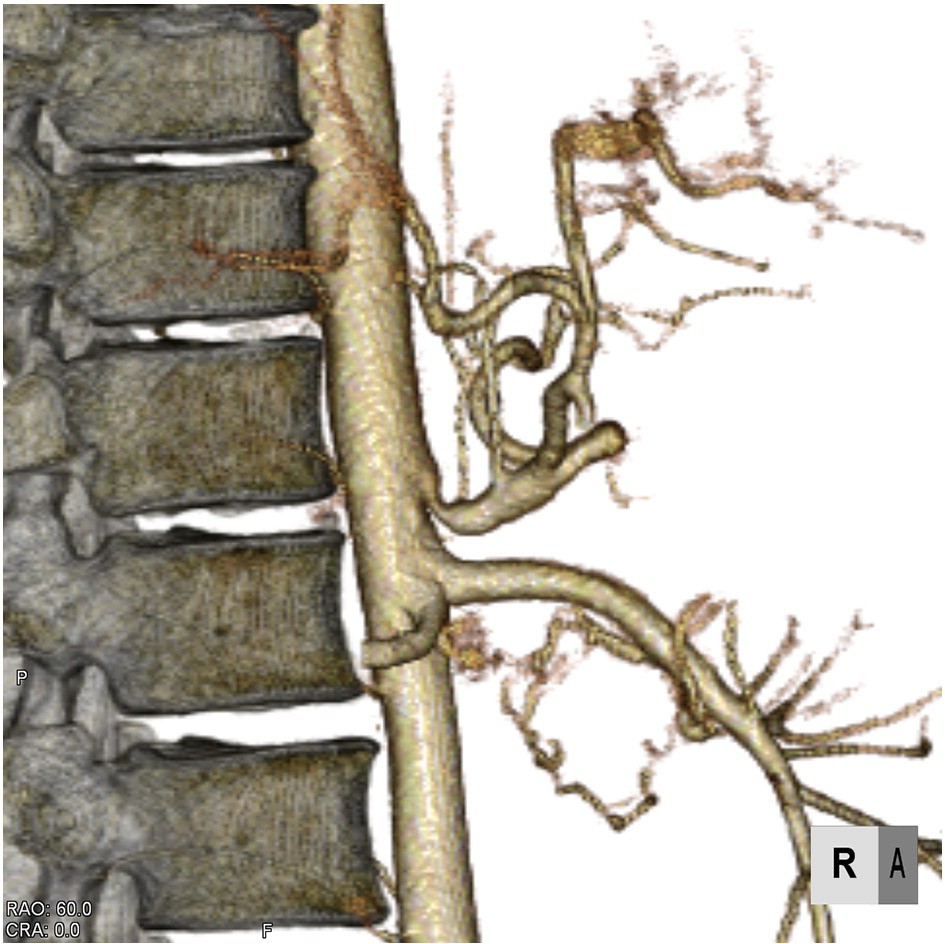
Fig. 3. Angiography of the SMA showing extravasation of the inferior pancreaticoduo- denal artery, and hepatic and splenic artery via a pancreaticoduodenal arcade.
Fig. 5. Celiac axis stenosis and dilated SMA.
On day 2, median arcuate ligament release and Damage control laparotomy using gauze packs were performed for the recurrent intra- abdominal bleeding. After successful removal of the packed gauze on day 4, oral intake and rehabilitation were initiated. On day 40, recurrent bleeding from the posterior superior pancreaticoduodenal artery required TAE using platinum coils. On day 47, because of perforation in the third portion of the duodenum, we performed a gastrojejunostomy and drainage followed by distal gastrectomy with Roux-en-Y reconstruction on day 99.
A 43-year-old man was admitted to the emergency department of the hospital because of sudden abdominal and back pain. He was healthy and without abdominal symptoms until the day of admission. Upon admission, his blood pressure was 95/45 mm Hg; pulse, 110 beats/min; and hemoglobin level, 9.2 g/dL. Initial fluid therapy with a
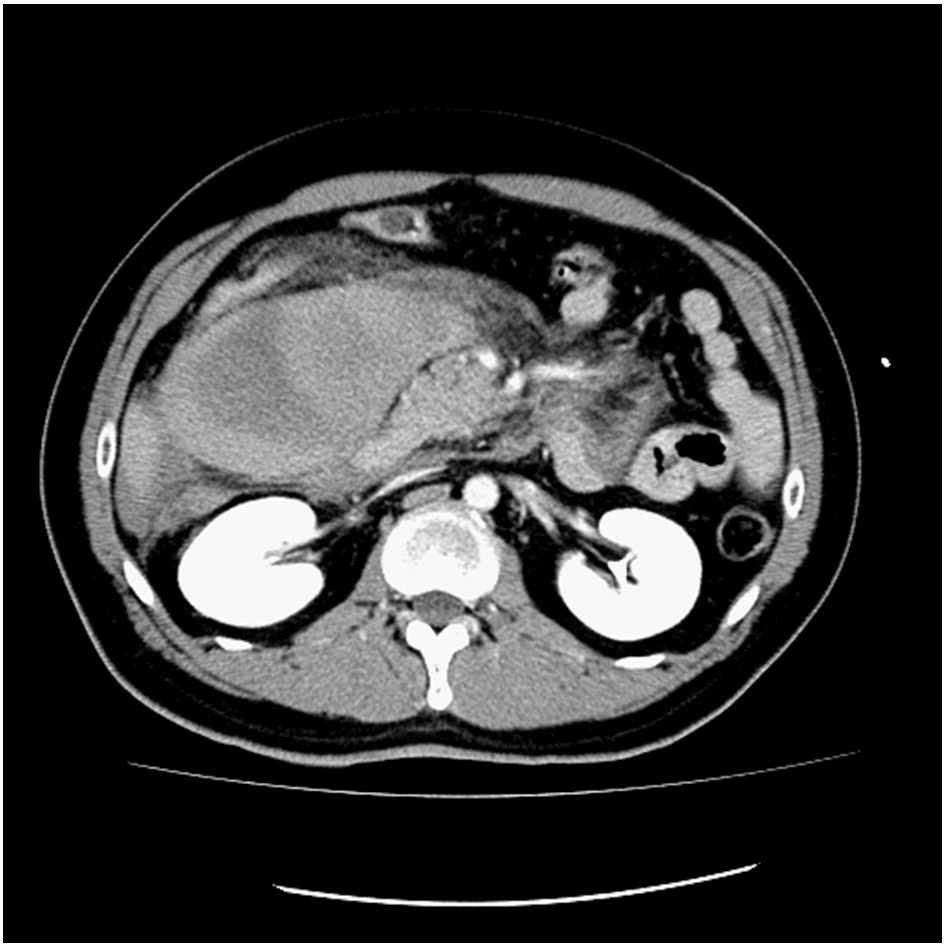
Fig. 4. Mesenteric hematoma of the Ascending colon without extravasation.
2-L crystalloid infusion reversed the hypotension. Abdominal con- trast-enhanced CT revealed a mesenteric hematoma without extrav- asation and focal narrowing of the celiac axis (Figs. 4 and 5). Angiography revealed a ruptured aneurysm, 4 mm in diameter, in the first branch of the jejunum artery as well as dilation of the SMA, first jejunal artery, and pancreaticoduodenal arcade (Figs. 6 and 7). The ruptured aneurysm was treated by TAE using platinum coils. On day 11, the patient was discharged. At the 6-month follow-up visit, no abdominal symptoms or aneurysm recurrence was observed.
A 56-year-old woman was transferred from another health care center to the emergency department of the hospital because of sudden-onset upper abdominal pain and intra-abdominal hemor- rhage. She was healthy until the day of admission. Upon admission, she had already received a 1-L crystalloid infusion and recovered

Fig. 6. Angiography of the SMA showing dilated superior mesenteric and pancreati- coduodenal arteries.
Y. Matsumura et al. / American Journal of Emergency Medicine 31 (2013) 1152.e1-1152.e4 1152.e3
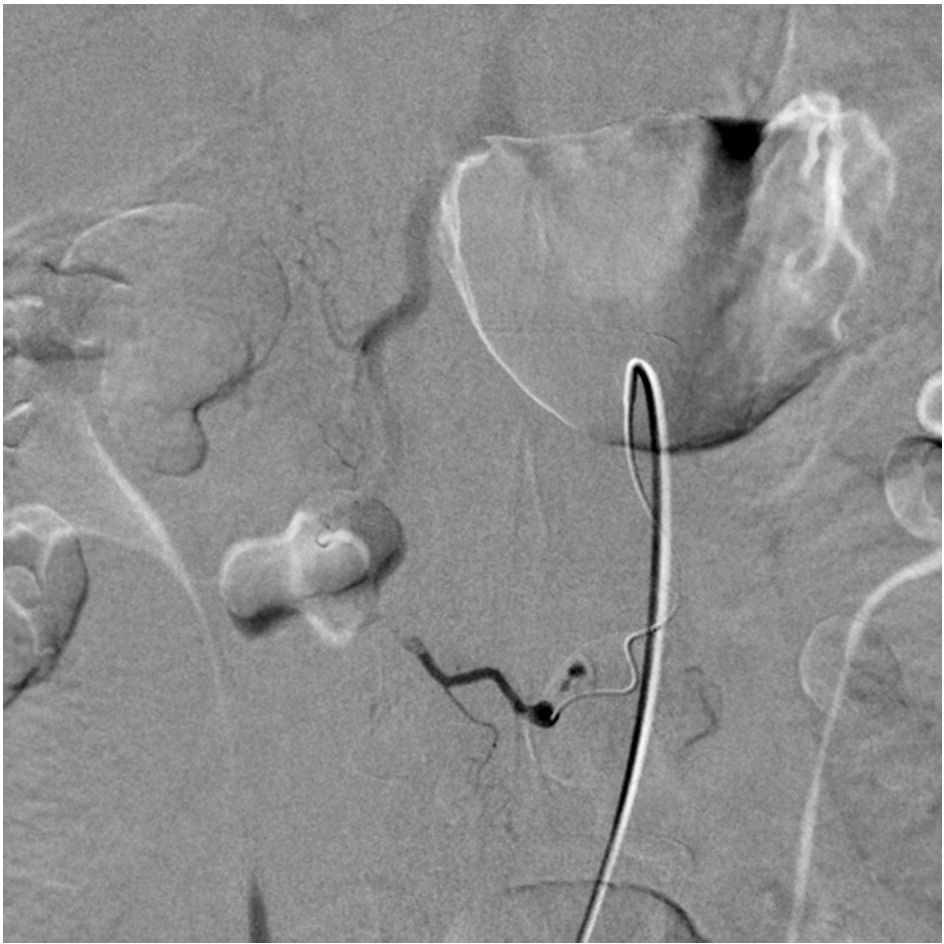
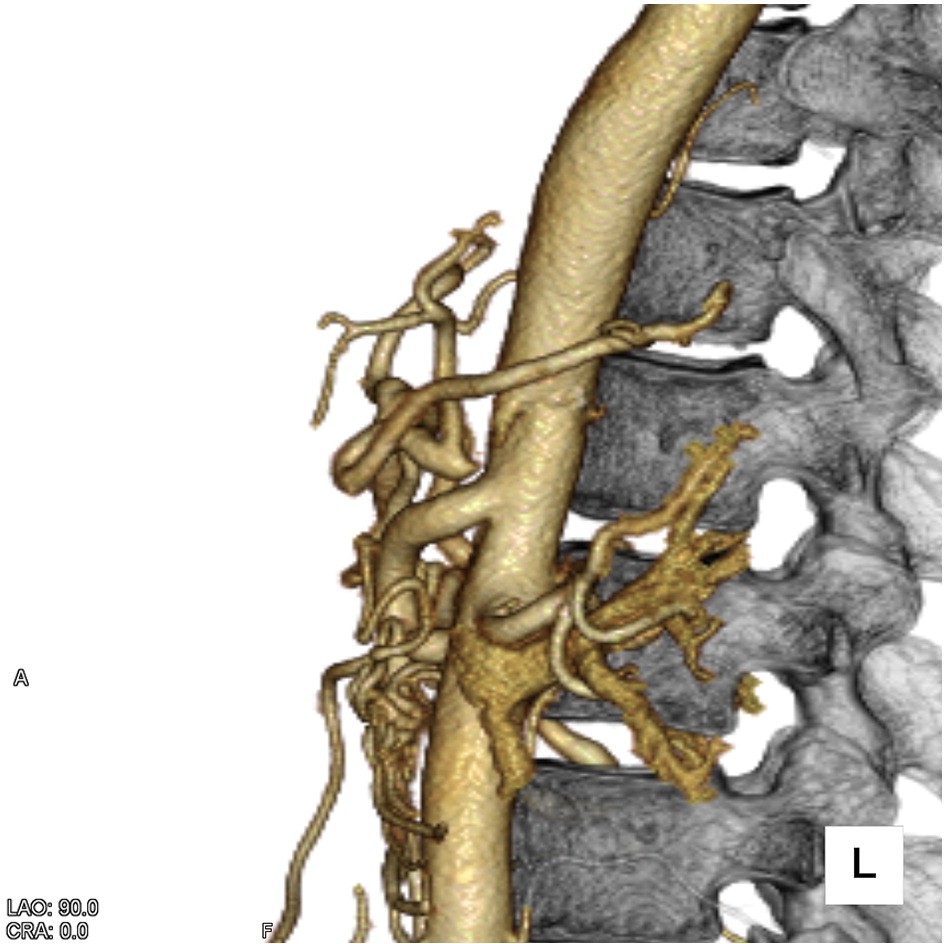
Fig. 7. Selective radiographic angiography showing a ruptured aneurysm of the first jejunal artery.
from the hypotension. Her blood pressure was 117/60 mm Hg; pulse, 80 beats/min; and hemoglobin level, 9.5 g/dL. Abdominal contrast- enhanced CT revealed a hematoma around the head of the pancreas and spleen and in the Douglas pouch without extravasation as well as focal occlusion of the celiac axis (Figs. 8 and 9). Angiography revealed a dilated pancreaticoduodenal arcade, suggestive of a ruptured pancreaticoduodenal artery aneurysm, but no aneurysm was detected (Fig. 10). On day 13, the patient was discharged. At the 2- month follow-up visit, she had no abdominal symptoms, and contrast-enhanced CT revealed no hematoma or pancreaticoduode- nal artery aneurysm.
Patients with median arcuate ligament syndrome often have eating-associated abdominal pain resulting in weight loss, but less frequently have pancreaticoduodenal artery aneurysms, which are
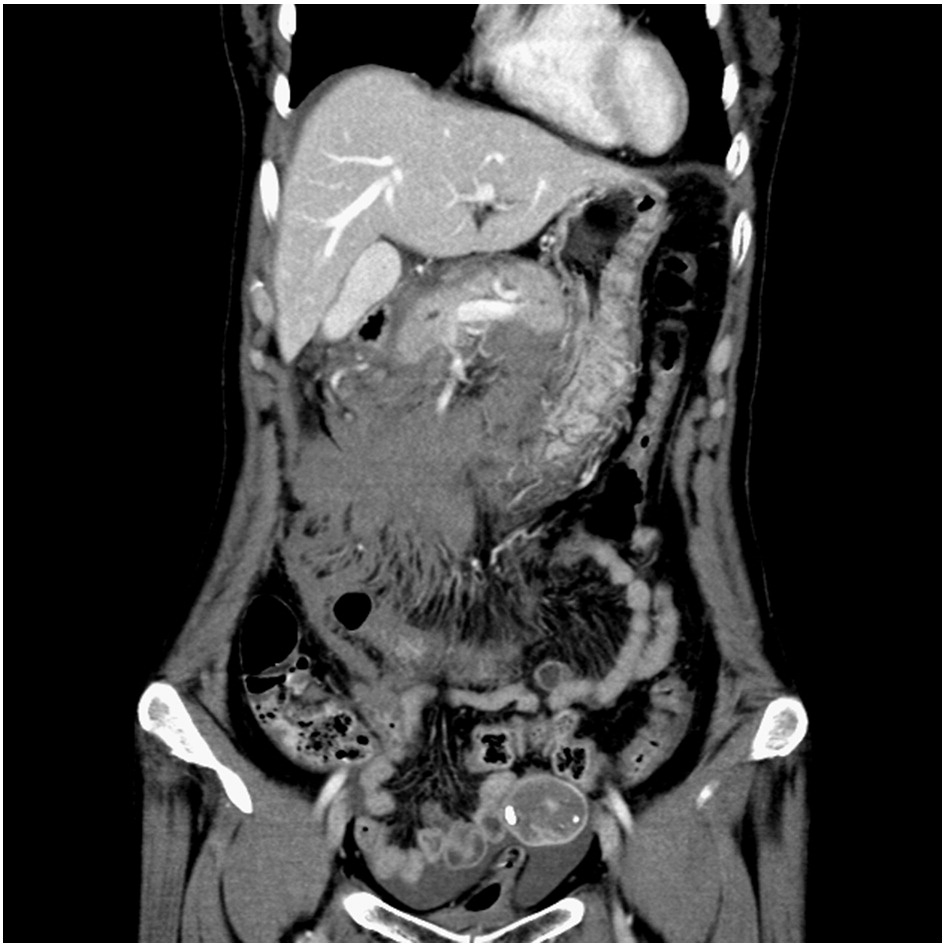
Fig. 8. Intra-abdominal hematoma without extravasation.
Fig. 9. Celiac axis occlusion and a dilated SMA.
known to be rare (2% of all visceral aneurysms) [3]. Rupture of pancreaticoduodenal artery aneurysms is reported to occur more often than ruptures of gastroduodenal artery aneurysms [4], but a small number of cases of hemorrhagic shock cases have been reported [5-7]. computed tomographic angiography has proved useful for detecting focal narrowing of the celiac axis [8], and the current report highlighted the use of 3-dimensional CT angiography to detect celiac stenosis. Selective angiographic embolization effectively treats rup- tured pancreaticoduodenal artery aneurysms [9]. We treated the pancreaticoduodenal artery aneurysms using coil embolization in case 1 (severe hemorrhagic shock) and case 2 (moderate hemorrhagic shock); both patients demonstrated celiac stenosis. Case 3 involved complete celiac occlusion, and severe hemorrhagic shock or aneu- rysms were not observed. Thus, celiac stenosis severity is not likely associated with hemorrhagic shock severity induced by ruptured aneurysms.
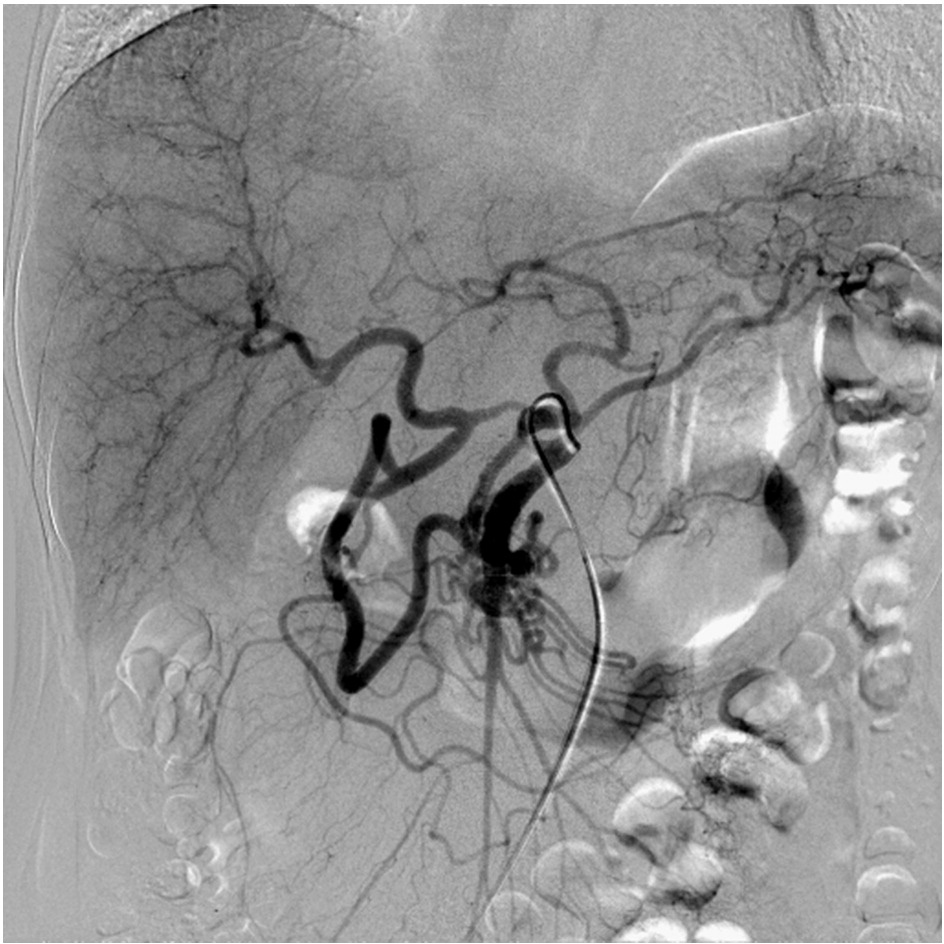
Fig. 10. Angiography of the SMA showing a dilated superior mesenteric and pancreaticoduodenal artery. No extravasation or aneurysm was detected.
1152.e4 Y. Matsumura et al. / American Journal of Emergency Medicine 31 (2013) 1152.e1-1152.e4
In conclusion, the results of the present study demonstrate that sudden-onset intra-abdominal hemorrhage of unknown etiology requires assessment for celiac artery stenosis using contrast- enhanced CT followed by angiography when median arcuate ligament syndrome is suspected.
Yosuke Matsumura MD Taka-aki Nakada MD, PhD Yoshiro Kobe MD, PhD Noriyuki Hattori MD, PhD Shigeto Oda MD, PhD
Department of Emergency and Critical Care Medicine Chiba University Graduate School of Medicine
Chuo, Chiba, Japan E-mail address: [email protected]
http://dx.doi.org/10.1016/j.ajem.2013.02.030
References
- Lindner HH, Kemprud E. A clinicoanatomical study of the arcuate ligament of the diaphragm. Arch Surg 1971;103:600-5.
- Snyder MA, Mahoney EB, Rob CG. Symptomatic celiac artery stenosis due to constriction by the neurofibrous tissue of the celiac ganglion. Surgery 1967;61:372-6.
- de Perrot M, Berney T, Deleaval J, et al. Management of true aneurysms of the pancreaticoduodenal arteries. Ann Surg 1999;229:416-20.
- Moore E, Matthews MR, Minion DJ, et al. Surgical management of peripancreatic arterial aneurysms. J Vasc Surg 2004;40:247-53.
- de Moya MA, Reisner AT, LaMuraglia GM, et al. Case records of the Massachusetts General Hospital. Case 1-2008. A 45-year-old man with sudden onset of abdominal pain and hypotension. N Engl J Med 2008;358:178-86.
- Flood K, Nicholson AA. Inferior pancreaticoduodenal artery aneurysms associated with occlusive lesions of the celiac axis: diagnosis, treatment options, outcomes, and review of the literature. Cardiovasc Intervent Radiol 2012 [in press].
- Ogino H, Sato Y, Banno T, et al. Embolization in a patient with ruptured anterior inferior pancreaticoduodenal arterial aneurysm with median arcuate ligament syndrome. Cardiovasc Intervent Radiol 2002;25:318-9.
- Horton KM, Talamini MA, Fishman EK. Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics 2005;25:1177-82.
- Bageacu S, Cuilleron M, Kaczmarek D, et al. True aneurysms of the pancreaticoduo- denal artery: successful non-operative management. Surgery 2006;139:608-16.
