An unusual cause of recurrent spontaneous pneumothorax: the Mounier-Kuhn syndrome
Contents lists available at ScienceDirect
American Journal of Emergency Medicine
journal homepage: www. elsevier. com/ locate/ajem
An unusual cause of recurrent Spontaneous pneumothorax: the Mounier-Kuhn syndrome?,??


Abstract
We present a case of 63-year-old man who was referred to the emergency department with a right-sided pneumothorax. He had a history of spontaneous pneumothorax for 2 times. The chest com- puted tomographic scan showed tracheobronchomegaly with an in- crease in the diameter of the trachea and right and left main bronchus. Fiberoptic bronchoscopy revealed enlarged trachea and both main bronchus with diverticulas. These findings are consistent with a diagnosis of Mounier-Kuhn syndrome. Mounier-Kuhn syndrome is a rare clinical and radiologic condition. It is character- ized by a tracheal and bronchial dilation. Diagnosis is made by com- puted tomography and bronchoscopy. Mounier-Kuhn syndrome should be kept in mind in the differential diagnosis of recurrent spontaneous pneumothorax.
Mounier-Kuhn Syndrome (MKS) or congenital tracheobronchomegaly is a rare clinical and radiologic condition. It is characterized by tracheal and bronchial dilation [1]. Tracheobronchomegaly was first reported by Czyhlarz in 1897 but is named after Mounier-Kuhn [2], who described the radiographic and bronchoscopic features of the syndrome in 1932. Its etiology remains uncertain, although there are occasional reports of a link with connective tissue disease. Histology shows loss of main airway smooth muscle and cartilage and associated tra- cheal diverticulosis. Dilatation of the trachea and proximal bronchi causes impaired secretion clearance, inefficient cough, persistent airway inflammation, and subsequent distal bronchiectasis and/or emphysema [3].
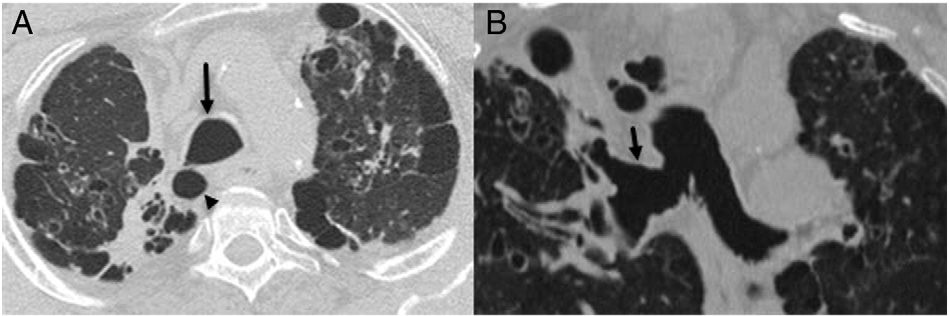
A 63-year-old man was referred to the emergency department with a right-sided pneumothorax. He had history of left spontaneous pneu- mothorax 33 years ago and right spontaneous pneumothorax 16 years ago. He had a smoking history of 60 packs per year and has been an exsmoker for 15 years. Enlargement of the trachea and a right-sided pneumothorax were detected in the chest radiograph (Fig. 1). The chest computed tomographic (CT) scan showed tracheabronchomegaly with an increase in the transverse diameter of the trachea and right and left main bronchus measured as 29, 23, and 20 mm, respectively (Fig. 2). Bronchiectasis and bullous emphysema were detected in the bilateral upper lobe, lower lobe superior, right middle lobe, and left lingula. Fiberoptic bronchoscopy revealed tracheal dilatation (Fig. 3A) and en- largement of both main bronchi. There were also multiple diverticula in both brochial system. Fig. 3B shows the right upper lobe diverticula.
? Conflict of interest: None of the authors has conflict of interest with the submission.
?? Financial support: No financial support was received for this submission.
These findings were consistent with a diagnosis of MKS. pulmonary function tests showed moderate airflow obstruction. We offered him medical therapy for chronic obstructive pulmonary disease and respiratory physiotherapy.
To the best of our knowledge, there are a few reports that regard MKS as a possible cause of spontaneous pneumothorax in the literature [4,5]. Most patients present with recurrent chest infections and copious purulent mucus production, whereas others present with wheezing or progressive exertional dyspnea [5].
Mounier-Kuhn syndrome has been described in virtually all age groups, with reported diagnoses in neonates and a 79-year-old woman [6] but generally presents in the third or fourth decade of life [5]. Our patient was close to old age.
Radiologic diagnosis can be established with plain chest radiograph alone. Woodring et al [7] published radiographic measurements of the trachea and proximal bronchi, which can be used to diagnose tracheobronchomegaly. Enlargement of the trachea was detected in the chest radiograph in our case.
Computed tomographic thorax may be required to confirm airway measurements and may additionally demonstrate associated pathology such as diverticula and bronchiectasis. In the current patient, the CT scan revealed enlargement of trachea, both main bronchus, and also bronchiectasis.
Bronchoscopy may show dilated proximal airways with associated dynamic collapse, purulent secretions, and tracheal diverticula. Recent data would suggest that bronchoscopy with confocal microscopy may aid diagnosis by permitting real-time analysis of the bronchial mucosal microstructure, demonstrating a deficiency of elastin fibres within the bronchial wall [8]. In our case, fiberoptic bronchoscopy revealed tracheal dilatation and enlargement of trachea, both main bronchi, and also multiple diverticula in both brochi system.
Lung function testing will generally show an obstructive pattern, with increased total lung capacity and residual volume consistent with air trapping. In the current case, pulmonary function tests showed moderate airflow obstruction.
asymptomatic patients may require no specific treatment. Other-
wise, the mainstay of therapy is the prevention and/or treatment of in- fectious complications, using methods such as effective clearance of secretions and antibiotic therapy. Tracheal stenting can improve symp- toms in patients with recurrent infections, severe dyspnea, and exercise limitation but can be associated with significant complications. Tracheobronchoplasty using a polypropylene mesh may improve symp- toms, quality of life scores, and exercise tolerance in selected patients [9]. Lung transplantation has been performed in at least 2 cases of MKS, one of who unfortunately died in the postoperative period [10].
0735-6757/(C) 2015
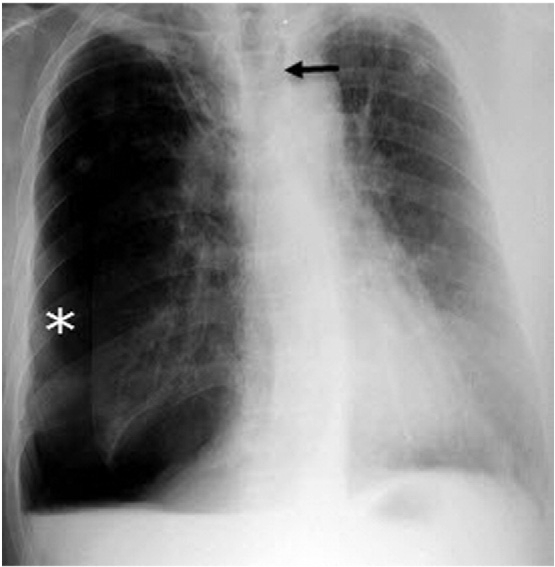 Fig. 1. Admission chest x-ray, demonstrating a right-sided pneumothorax (star) and dilated trachea (arrow).
Fig. 1. Admission chest x-ray, demonstrating a right-sided pneumothorax (star) and dilated trachea (arrow).
We offer him medical therapy for chronic obstructive pulmonary disease (COPD) and respiratory physiotherapy.
As a result, MKS should be kept in mind in the differential diagnosis of recurrent spontaneous pneumothorax.
Elif Nisa Unlu, MD*
Department of Radiology, Faculty of Medicine, Duzce University,
*Corresponding author. Duzce Universitesi Tip Fakultesi Radyoloji Anabilim Dali Konuralp Yerleskesi, TR-81000, Duzce, Turkey
Tel.: +90 542 14 16; fax: +90 542 13 02
E-mail address: [email protected]
Ali Nihat Annakkaya, MD Ege Gulec Balbay, MD Leyla Yilmaz Aydin, MD
Sinem Safci, MD
Department of Chest Diseases, Faculty of Medicine, Duzce University,
Duzce, Turkey E-mail addresses: [email protected], [email protected], [email protected], [email protected]
Fig. 3. Bronchoscopic views show a dilated trachea (A) and right upper lobe diverticula (B).
Mertay Boran, MD
Department of Thoracic Surgery, Faculty of Medicine, Duzce University,
Duzce, Turkey E-mail address: [email protected]
Derya Guclu, MD
Department of Radiology, Duzce Ataturk State Hospital, Duzce, Turkey
E-mail address: [email protected]
http://dx.doi.org/10.1016/j.ajem.2015.05.050
References
- Simon M, Vremaroiu P, Andrei F. Mounier-Kuhn syndrome. J Bronchol Interv Pulmonol 2014;21(2):145-9. http://dx.doi.org/10.1097/LBR.0000000000000068.
- Mounier-Kuhn P. Dilatation de la trachee: constatations radiographiques et
bronchoscopiques. Lyon Med 1932;150:106.
Schwartz M, Rossoff L. Tracheobronchomegaly. Chest 1994;106:1589-90.
- Tschopp JM, Rami-Porta R, Noppen M, Astoul P. Management of spontaneous pneumothorax: state of the art. Eur Respir J 2006;28:637-50.
- Kent BD, Sulaiman I, Akasheh NB, Nadarajan P, Moloney E, Lane SJ. An unusual cause
of spontaneous pneumothorax: the Mounier-Kuhn syndrome. Ir Med J 2011;104(5): 152-3.
Falconer M, Collins DR, Feeney J, Torreggiani WC. Mounier-Kuhn syndrome in an older patient. Age Ageing 2008;37:115-6.
- Woodring JH, Howard II RS, Rehm SR. Congenital tracheobronchomegaly: a report of
10 cases and review of the literature. J Thorac Imaging 1991;6:1-10.
Thiberville L, Moreno-Swirc S, Vercauteren T, Peltier E, Cav C, Bourg Heckly G. In vivo imaging of the bronchial wall microstructure using fibered confocal fluorescence microscopy. Am J Respir Crit Care Med 2007;175:22-31 [1991; 6:1-10].
- Majid A, Guerrero J, Gangadharan S, Feller-Kopman D, Boiselle P, DeCamp M, et al. Tracheobronchoplasty for severe tracheomalacia. Chest 2008;134:801-7.
- Minai O, Mehta AC, Pettersson G, Demet K. Lung transplantation in a patient with
Mounier-Kuhn syndrome. J Thorac Cardiovasc Surg 2006;132:737-8.

Fig. 2. Axial CT image (A), demonstrating tracheomegaly (arrow), large Tracheal diverticulum (arrowhead), and severe paraseptal emphysema. Coronal reformatted CT image (B) shows dilatation of right main bronchus (arrow).