Advanced airway management in out of hospital cardiac arrest: A systematic review and meta-analysis
a b s t r a c t
Objectives: To assess the difference in Survival and neurological outcomes between Endotracheal tube intu- bation and Supraglottic airway devices used during out-of-hospital cardiac arrest (OHCA).
Methods: A systematic search of five databases was performed by two independent reviewers until September 2018. Included studies reported on (1) OHCA or cardiopulmonary resuscitation, and (2) endotracheal intubation versus supraglottic airway device intubation. Exclusion criteria (1) stimulation studies, (2) selectively included/ excluded patients, (3) in-hospital cardiac arrest. Odds Ratios (OR) with random effect modelling was used. Pri- mary outcomes: (1) return of spontaneous circulation (ROSC), (2) Survival to hospital admission, (3) survival to hospital discharge, (4) discharge with a Neurologically intact state.
Results: Twenty-nine studies (n = 539,146) showed that overall, ETT use resulted in a heterogeneous, but signif- icant increase in ROSC (OR = 1.44; 95%CI = 1.27 to 1.63; I2 = 91%; p b 0.00001) and Survival to admission (OR = 1.36; 95%CI = 1.12 to 1.66; I2 = 91%; p = 0.002). There was no significant difference in survival to discharge or neurological outcome (p N 0.0125). On sensitivity analysis of RCTs, there was no significant difference in ROSC, survival to admission, survival to discharge or neurological outcome (p N 0.0125). On analysis of automated chest compression, without heterogeneity, ETT provided a significant increase in ROSC (OR = 1.55; 95%CI = 1.20 to 2.00; I2 = 0%; p = 0.0009) and survival to admission (OR = 2.16; 95%CI = 1.54 to 3.02; I2 = 0%; p b
0.00001).
Conclusions: The overall heterogeneous benefit in survival with ETT was not replicated in the low risk RCTs, with no significant difference in survival or neurological outcome. In the presence of automated chest compressions, ETT intubation may result in Survival benefits.
(C) 2018
Introduction
Out of Hospital Cardiac Arrest (OHCA) is the third leading cause of death in the United States and represents a significant Public health concern [1]. OHCA is a heterogeneous and time critical condition with a variety of aetiologies, and little is known about the benefits of various interventions [2]. Previous guidelines have reduced the emphasis on en- dotracheal intubation as an airway Management strategy, although op- timal airway management remains uncertain [2].
* Corresponding author at: School of Medicine, University of Queensland, A: 12 Macon St, Birtinya, QLD 4575, Australia.
E-mail address: [email protected] (L. White).
advanced airway management strategies for OHCA include endotra- cheal tube (ETT) intubation or use of Supraglottic airway devices. ETT intubation is traditionally considered a definitive airway, although greater skill is required for its placement and the process of securing the airway may be associated with unrecognized misplacement of the tube, increased number of attempts and interruptions to chest compres- sions [3,4]. Since previous meta-analyses [5], a number of studies have renewed interest in establishing optimal airway management strategies for OHCA [6-8].
The aim of this study is to perform the most thorough and up to date systematic review and meta-analysis to assess the difference in survival and neurological outcomes between ETT intubation and SGA devices for advanced airway management in OHCA.
https://doi.org/10.1016/j.ajem.2018.09.045
0735-6757/(C) 2018
L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306 2299
Methods
This study was registered with the International Prospective Regis- ter of Systematic Reviews (PROSPERO; CRD42018100126). The Pre- ferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was followed.
Search strategy
A systematic search was performed by two independent reviewers (LW & RV). The search included SCOPUS, PubMed, Medline, Cochrane Central Register of Controlled Trials and Web of Science. This search was conducted from the inception of the databases until September 2018. The search was performed using Medical Subject Headings (MeSH) terms, which included: “Airway management” plus “cardiac ar- rest”; “Emergency Medical Service” plus “out-of-hospital cardiac arrest” plus “airway management”. The term “Airway Management” consists of MeSH terms “intubation”, “laryngeal mask” and “positive pressure res- piration”. “Emergency Medical Service” consists of MeSH terms “ambu- lance” and “prehospital emergency care“. For completeness, a manual reference check of a recent review (5) and other accepted papers was performed to identify any additional studies.
Eligibility criteria
For a study to be included in this meta-analysis the authors were re- quired to report on (1) cardiac arrest or cardiopulmonary resuscitation
(2) endotracheal intubation versus supraglottic airway device intuba- tion. Supraglottic airway devices included laryngeal masks and laryn- geal tubes. Clinical outcomes of interest were required to be presented (no systematic review or meta-analysis). Only out of hospital cardiac ar- rest studies were eligible for inclusion. Two reviewers (LW & RV) assessed agreed upon each study for inclusion in this systematic review. All study designs were eligible for inclusion.
Exclusion criteria
Manikin and simulation studies were excluded. Studies that selec- tively included or excluded patients were ineligible, for example witnessed cardiac arrest patients. In hospital cardiac arrests were not el- igible for inclusion.
Outcomes
The primary outcomes of interest included (1) return of spontane- ous circulation (ROSC) (2) survival to hospital admission (3) survival to hospital discharge (4) survival to discharge with a cognitively intact state. An intact neurological state was defined as a cerebral performance category one or two or Modified Rankin scale <= 3. All included studies were screened for additional common outcomes for post hoc analysis.
Data collection and extraction
Two reviewers (LW and RV) independently extracted data from each article that met the inclusion criteria. The data extracted from each study included the study design, sample size, airway device, cause of cardiac arrest, registry utilized and outcome measures. The data collected by each reviewer was then compared for homogeneity.
Risk of bias
Two independent reviewers assessed each study for risk of bias. Two separate tools were used. Randomised controlled trials (RCTs) were assessed for risk of bias and methodological quality using the Cochrane Collaboration’s tool for assessing the risk of bias [9]. Non-randomised were assessed using the ROBINS-I tool [10].
Statistical analyses
The combined data was analysed using RevMan 5.3 software (The Nordic Cochrane Centre, Copenhagen, Denmark). Dichotomous out- comes were analysed using an Odds Ratio (OR) with 95% confidence in- terval (CI). The Mantel-Haenszel (M-H) random effects model was used. The absolute difference between the two groups was measured utilizing the Risk difference with 95%CIs. Heterogeneity was assess using the I2 statistic, with an I2 N 50% indicating significant heterogene- ity. Given we intended to assess four outcome measures, we used the Bonferroni method to minimise the risk of type one errors. Therefore a p value of b0.0125 provided evidence of significant OR.
Subgroup and sensitivity analyses
Pre-specified sensitivity analyses were performed based on care provider, manual chest compressions, automatic chest compressions, laryngeal mask use, laryngeal tube use, cause of arrest, location of arrest and study quality. In the case of studies utilizing duplicate databases, two authors (LW & RV) independently decided which duplicates to ex- clude on sensitivity analysis. Any disagreements were settled by a third reviewer (TM).
Assessment of quality of evidence
The quality of evidence and confidence in estimates of effect were assessed using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach [11]. This approach was per- formed by considering the within study risk of bias, heterogeneity be- tween studies, effect estimate precision and the risk of publication bias. Publication bias and small-study effects were assessed via funnel plots of standard errors versus effect estimates. This study was written in accordance with the Meta-analysis Of Observational Studies in Epide- miology (MOOSE) checklist [12].
Results
Literature search results
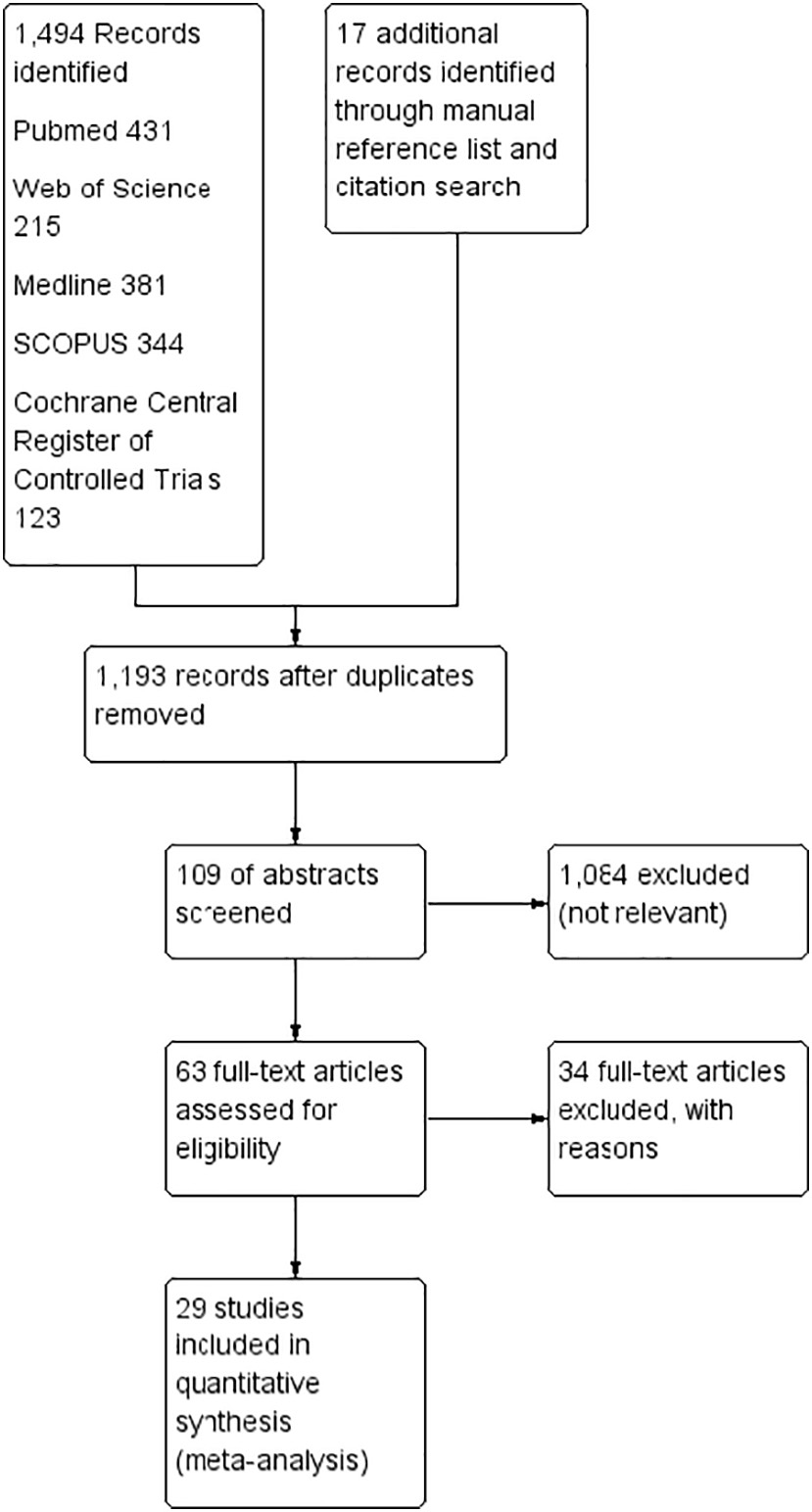
The systematic literature search yielded 29 studies for inclusion in this meta-analysis (Fig. 1). The initial electronic search identified 1494 studies and a further 17 were identified on manual reference and cita- tion searches. Following the removal of duplicate records and title screening, 109 abstracts were reviewed. Sixty-three full text studies were reviewed to identify the 26 included studies. There were no dis- agreements between the two authors performing the search review. In total data from 539,146 patients were included (Table 1). Details on the individual excluded studies are listed in Table S1 [13-48].
Risk of bias
Each study was then screened for risk of bias and methodological quality using the Cochrane Collaboration’s tool for assessing the risk of bias for RCTs and the ROBINS-I tool for non-randomised studies (Table S2). Included in this meta-analysis were five low risk RCTS, eight moderate risk non-randomised studies and sixteen serious risk non-randomised studies.
Database duplication and outcome measures
Of the twenty-six studies included, eight overlapping registry trials were found. Various studies performed in Japan were included in this meta-analysis [6,31,56,58,63,66,67,69]. However, due to the time span of the Fukuda et al. study (2005-2014 inclusive), which included Japan-wide data, some studies [31,58,63,67,69] were omitted to avoid the duplication of information. Despite taking place within the same
2300 L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306
 heterogeneity on analysis of low risk RCTs (OR = 0.92; 95%CI = 0.80 to 1.05; I2 = 23%; p = 0.22).
heterogeneity on analysis of low risk RCTs (OR = 0.92; 95%CI = 0.80 to 1.05; I2 = 23%; p = 0.22).
Survival to admission
Fourteen studies (n = 51,756) investigated survival to admission, with a significant increase with ETT (OR = 1.36; 95%CI = 1.12 to 1.66; I2 = 91%; p = 0.002; Table 3) [7,14,49,50,52,53,55,58-61,64,70,71]. The
funnel plot of the overall result was skewed to the right (Fig. S2). Based on the GRADE framework this was judged to be very low quality evi- dence. There was no change in significance or heterogeneity with removal of duplicate databases. On sensitivity analysis for resuscitation variables LMA and laryngeal tube, there was no significant difference with signifi- cant heterogeneity (Table 3). Without significant heterogeneity, there was a significant increase in survival to admission with ETT during auto- mated chest compressions (OR = 2.16; 95%CI = 1.54 to 3.02; I2 = 0%; p b 0.00001). On analysis of the low risk RCTs there was no significant difference between ETT and SGA (OR = 0.97; 95%CI = 0.68 to 1.09; I2 = 0%; p = 0.59).
Survival to discharge
Fig. 1. Study identification algorithm. This diagram outlines the filtering process from the literature search through to study inclusion.
time span as the Fukuda study, studies by Hasegawa et al. and Takei et al. were included within the subgroup analysis. These studies pro- vided information regarding patient ROSC prior to hospital arrival, and also additional data from the 2004 to 2005 period, respectively. Within each subgroup analysis the omitted studies from overlapping registries were eligible for inclusion if in lieu of results from Fukuda et al. or Hasegawa et al. and Takei et al. All studies were individually screened and no additional outcomes were identified for post-hoc analysis.
ROSC
Twenty-three studies (n = 397,158) investigated the effect of ad- vanced airway management on ROSC showing a significant increase with ETT (OR = 1.44; 95%CI = 1.27 to 1.63; I2 = 91%; p b 0.00001;
Table 2) [6,7,14,31,47,49-53,55-59,61-70,72]. The funnel plot of the overall result was skewed to the right (Fig. S1). Based on the GRADE framework this was judged to be very low quality evidence. There was no change in significance or heterogeneity with removal of dupli- cate databases. On subgroup analysis for resuscitation variables EMT provider and manual chest compressions remained significantly in fa- vour of ETT (p b 0.0125) with significant heterogeneity. The only out- come to have a significant increase in ROSC without heterogeneity was cardiac arrest using automated chest compressions (OR = 1.55; 95%CI = 1.20 to 2.00; I2 = 0%; p = 0.0009). On analysis of moderate and serious risk studies, the significant benefit of ETT with significant heterogeneity remained. The significant effect was lost without
Twenty-two studies (n = 440,564) investigated survival to dis- charge with no significant difference with ETT compared to SGA (OR = 1.28; 95%CI = 1.02 to 1.60; I2 = 96%; p = 0.03; Table 4)
[6,7,14,47,50-58,60,61,63,65-68,70-72]. The funnel plot of the over- all result was skewed to the right (Fig. S3). Based on the GRADE framework this was judged to be very low quality evidence. There was no change in significance or heterogeneity with removal of du- plicate databases. The subgroup analysis there was no change in non-significance with Laryngeal tubes, whereas the LMA subgroup had reached significance over ETT with heterogeneity (OR = 1.80; 95%CI = 1.14 to 2.83; I2 = 85%; p = 0.01) (Table 4). Subgroup anal- ysis for automated chest compressions was unable to be performed. There was no significant difference in survival to discharge in the low risk RCTs (OR = 0.90; 95%CI = 0.68 to 1.20; I2 = 70%; p = 0.49;
Table 4).
Survival to discharge with a neurologically intact state
Fourteen studies (n = 438,261) showed no significant difference (p N 0.0125) in discharge with a neurologically intact state (p = 0.16; Table 5) [6,7,47,51,56,58,59,61,63,65,67,68,70,72]. The funnel plot of
the overall result was skewed to the right (Fig. S4). Based on the GRADE framework this was judged to be very low quality evidence. This remained unchanged based on removal of duplicate studies, EMT provider, manual chest compressions, LMA use and laryngeal tube use (Table 5). When separated into low, moderate and serious risk studies, the effect remained non-significant.
Discussion
This was the largest and most up to date systematic review and meta-analysis on airway management in OHCA, with 29 studies and 539,146 patients included. Overall, ETT demonstrated better early sur- vival rates (ROSC and survival to admission) than SGA devices. Despite the improved early survival rates, there was no significant in longer term outcomes such as survival to discharge and neurological function at discharge from hospital. The clinical application of the overall im- provements in early survival with the use of ETT is limited due to the significant heterogeneity (I2 = 91%). This reflects the multifactorial na- ture of both cardiac arrest aetiology and management. For this reason multiple sensitivity analyses were performed.
The first sensitivity analysis performed was to control for the skill level of care providers, thus an analysis including EMT providers was undertaken. Again, the initial overall increase in early survival outcomes
L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306
2301
Study characteristics.
|
Study |
Study design |
Sample (ETT/SGA) |
Cause of OOHCA |
SGA employed |
Registry utilized (year) |
Outcomes |
Risk of bias? |
|
Becker et al. [49] |
Retrospective Cohort |
126 (84/42) |
All causes |
Not specified |
N/A |
ROSC |
Serious |
|
Benger et al. [14] |
RCT |
615 (209/406) |
Non-traumatic |
i-Gel, LMA Supreme |
N/A |
ROSC |
Low |
admission
3. Survival to discharge
|
Benger et al. [70] |
RCT |
9296 |
Non-traumatic |
i-Gel |
N/A |
1. ROSC |
Low |
|
(4410/4886) |
1. Survival to |
||||||
|
Bernhard et al. |
Retrospective |
22,350 |
All causes |
Not specified |
German Resuscitation Registry (2010-2016) |
admission 2. Survival to discharge 2. Neurological outcome 3. ROSC |
Moderate |
|
[7] |
cohort |
(17,887/4363) |
4. Survival to admission |
||||
|
Cady et al. [50] |
Retrospective |
5822 |
All causes |
Combitube |
N/A |
5. Survival to discharge 6. Neurological outcome 1. ROSC |
Serious |
|
cohort |
(4335/1437) |
2. Survival to admission 3. Survival to |
|||||
|
Chiang et al. [51] |
Retrospective |
4640 |
Non-traumatic |
Not specified |
Utstein style registry, Taipei (2008-2013) |
discharge 3. ROSC |
Serious |
|
Davey & Dicker |
cohort Retrospective |
(1541/3099) 965 (293/672) |
All causes |
Not specified |
St John New Zealand OHCA (2013-2015) |
Survival toadmission Survival to discharge1. ROSC |
Serious |
|
[52] cohort Do Shin et al. [53] Retrospective |
641 (250/391) |
Presumed cardiogenic aetiology |
Not specified |
Korea nationwide OHCA cohort database (2006-2008) |
2. Survived to admission 3. Survival to discharge 1. Survival to |
Moderate |
|
|
cohort |
admission |
||||||
|
2. Survival to discharge |
|||||||
|
Evans et al. [54] Erath et al. [71] |
Retrospective cohort Propensity matched |
1555 (1282/273) 208 (160/48) |
Traumatic All causes |
Not specified Laryngeal tube |
Resuscitation outcomes Consortium epistry-trauma and prospective observational prehospital and hospital registry (2005-2007 & 2010-2011) N/A |
1. Survival to discharge 1. Survival to |
Serious Moderate |
|
cohort |
admission 2. Survival to |
||||||
|
Fukuda et al. [6] |
Retrospective |
132,874 |
All causes |
Not specified |
All Japan Utstein Registry (2005-2014) |
discharge 3. Survival to |
Moderate |
|
cohort |
(22,806/110,068) |
discharge |
|||||
(continued on next page)
Table 1 (continued)
2302
L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306
|
Study |
Study design |
Sample (ETT/SGA) |
Cause of OOHCA |
SGA employed |
Registry utilized (year) |
Outcomes |
Risk of bias? |
|
Hanif et al. [55] |
Retrospective |
1158 (1027/131) |
All causes |
Combitube or |
N/A |
4. Neurological outcome 1. ROSC |
Moderate |
|
cohort |
oesophageal obturator |
2. Survival to admission 3. Survival to discharge |
|||||
|
Hasegawa & |
Retrospective |
281,522 |
All causes |
Not specified |
All-Japan Utstein Registry (2005-2014) |
1. ROSC |
Serious |
|
Takei [56] Jarman et al. [57] |
cohort Prospective |
(41,972/239,550) 316 (273/43) |
All causes |
King LT |
N/A |
2. Survival to discharge 3. Neurological outcome 1. ROSC |
Moderate |
|
Kajino et al. [58] |
observational Retrospective |
5377 |
Non-traumatic |
Not specified |
Utstein style registry, Osaka (2005-2008) |
1. ROSC |
Serious |
|
Kang et al. 2015 |
cohort Retrospective |
(1679/3698) 2829 |
Non-traumatic |
Not specified |
Korea nationwide OHCA cohort database (2010-2013) |
Survival to admission |
Serious |
|
[59] |
cohort |
(1634/1195) |
2. Survival to |
||||
|
Lin et al. [60] |
Retrospective |
1428 (1384/44) |
All causes |
Not specified |
Taiwan EMS and hospital registries |
discharge 3. Neurological outcome 1. ROSC |
Serious |
|
cohort |
2. Survival to admission 3. Survival to |
||||||
|
McMullan et al. |
Retrospective |
8701 |
All causes |
Not specified |
CARES Registry (2011) |
discharge 1. ROSC |
Moderate |
|
[61] |
cohort |
(5591/3110) |
Survival to admissionoutcome |
||||
|
Mulder et al. [62] |
RCT |
188 (101/87) |
Non-traumatic |
LMA |
N/A |
ROSC |
Low |
|
Nagao et al. [31] |
Retrospective |
199 (10/189) |
All causes |
LMA and combitube |
Utstein style registry, Tokyo (2006-2007) |
ROSC |
Serious |
|
Noda et al. [63] |
cohort Retrospective |
28 (4/24) |
Cardiogenic aetiology |
LMA and combitube |
Utstein style registry, Kyushu University Hospital (2000-2006) |
ROSC |
Serious |
|
cohort |
Survival to admissiondischarge |
||||||
|
Rabitsch et al. |
RCT |
172 (83/89) |
Non-traumatic |
Combitube |
N/A |
4. Neurological outcome 1. ROSC |
Low |
|
[64] |
2. Survival to admission 3. Survival to discharge |
||||||
|
Sulzgruber et al. [65] |
Propensity matched analysis |
420 (210/210) |
All causes |
Not specified |
N/A |
1. Survival to discharge |
Moderate |
L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306 2303
* Randomised controlled trials (RCTs) were assessed for risk of bias and methodological quality using the Cochrane Collaboration’s tool for assessing the risk of bias [9]. Non-randomised were assessed using the ROBINS-I tool [10]. ROSC = return of spontaneous circulation; OHCA = out-of-hospital cardiac arrest; ETT = endotracheal tube; SGA = supraglottic airway; LMA = laryngeal mask airway; LT = Laryngeal Tube.
but not survival to discharge or neurological state with ETT insertion remained. This sensitivity analysis still had significant limitations such as, difference in seniority and skill level of EMT, indication and airway difficulty. All of these factors directly impact on the success of the airway techniques, as well as, the expertise of the provider managing the car- diac arrest as a whole [73]. Furthermore, the majority of studies did not report on intervention crossover rates, which would adversely affect time to successful ventilation, as well as delays to chest compressions and other interventions. A further limitation to the overall results in- clude large amount of overlapping data from the same databases. When studies were assessed for duplication, eight overlapping studies were identified. On sensitivity analysis, duplicate databases were re- moved which resulted in no change the significance of the overall re- sults, or the heterogeneity of the overall results.
2. Neurological outcome
ROSC
Serious
Serious
Serious
Low
Serious
Serious
Recommendations based on prior meta-analyses have been largely limited by the quality of included studies. For the first time, the present study performed a sensitivity analysis based on low risk of bias RCTs. The sensitivity analyses showed no difference between ETT and SGA in regard to ROSC (OR = 0.90; 95%CI = 0.65 to 1.25; I2 = 12%; p =
Utstein style registry, Ishikawa (2004-2008)
Modified Upstein style registry, Saitama (2006-2007)
0.59), survival to admission (OR = 1.00; 95%CI = 0.68 to 1.47; I2 = 0%; p = 0.99), survival to discharge (OR = 0.90; 95%CI = 0.68 to 1.20; I2 = 70%; p = 0.49) or neurological recovery at discharge (OR = 0.88; 95%CI = 0.57 to 1.35; I2 = 84%; p = 0.55). All five studies were rel- atively homogenous utilizing non-physician providers for the manage- ment of non-Traumatic cardiac arrest. Three [52,63] of the five studies compared ETT to LMA, whereas the studies by Wang et al. and Rabitsch et alcompared ETT to esophagotracheal combitube (ETC). Between the studies, the first attempt success rate for LMA (Supreme and I-gel) in- sertion was reasonably consistent (75-79%). There was a higher than expected First attempt success rate for ETC 98% and wide variation in ETT first attempt success rate (51-96%). Each of these studies appears to have controlled for intra and post resuscitation care by following na- tional guidelines. However, adherence to these guidelines is not commented on. Notably, none of these studies included patients receiv- ing automated chest compressions. Therefore, these five RCTs serve as the first level 1 recommendation to show no difference in survival or neurological outcome between ETT and SGA in advanced airway man- agement for OHCA.
Not specified
LMA and combitube
All-Japan Utstein Registry (2005-2007)
King laryngeal tube, LMA and combitube Laryngeal tube
ROC PRIMED Trial
N/A
Not specified
Marshall LMA
(2008-2011)
Further sensitivity analyses were performed in an attempt to control for specific intra-arrest management variables. These included analyses of SGA device type and type of chest compression. Interestingly, the only management related sensitivity analysis to show a significant ben- efit without heterogeneity was in the presence of concurrent automated chest compressions. This is important given the increasing popularity of automated compression devices for both in and out of hospital cardiac arrest [7,14]. This subgroup analysis was only able to be performed on short term outcomes (ROSC and survival to admission).
All causes (cardiac and non-cardiac subgroups)
Non-traumatic
Non-traumatic
Non-traumatic
All causes (traumatic and non-traumatic subgroups)
All causes
Analyses of intrathoracic pressure during both manual and auto- mated chest compressions have previously been performed [74]. These show that there a greater sustained pressure throughout the chest compression cycle with mechanical compressions [75]. However, compression induced ventilation is not possible in humans. Therefore, a patent airway and assisted ventilation is still required during cardiopul- monary resuscitation. The benefit of ETT over SGA in this setting is likely related to elevated intrathoracic pressure and thus reduced efficacy of SGAs. These findings suggest that if an emergency response service uti- lizes automated compression devices, Endotracheal tubes are likely to result in increased survival. The one caveat to this suggestion is that when mechanical compressions are used, the placement of an ETT will be more difficult. For this reason, airway adjuncts such as the digitally- assisted pre-loaded bougie technique should be used [76,77].
Takei et al. [66]
Prospective observational
948 (268/680)
Tanebe et al. [67]
Retrospective cohort
42,632 (12,992/29,640)
Wang et al. [68]
Secondary analysis of RCT data
RCT
10,425 (8487/1968) 3000 (1495/1505)
Wang et al. [73]
Yanagawa & Sakamoto [47]
Retrospective
636 (158/478)
Yeung et al. [69]
Prospective observational
75 (50/25)
Airway management is only one facet of intra and post cardiopulmo- nary resuscitation care. For this reason, it is understandable why any dif- ference in outcome will diminish over time. The results of the present study showed no significant increase in survival to discharge or neuro- logical outcome, with significant heterogeneity on all subgroup
2304 L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306
Table 2
Association between Endotracheal tube intubation versus Supraglottic airway for return of spontaneous circulation (ROSC) during cardiopulmonary resuscitation.
Group Events/total no of patients Risk difference, % (95%CI) Relative odds I2%
|
ETT |
SGA |
Odds ratio (95%CI) |
p value |
|||
|
18,877/95,314 |
20,942/301,844 |
0.05 (0.03 to 0.06) |
1.44 (1.27 to 1.63) |
b0.00001 |
91 |
|
|
Analysis after duplicate database removal [6,7,14,49-57,59-66,68,69,70,72] |
17,201/80471 |
17,835/263513 |
0.05 (0.03 to 0.08) |
1.36 (1.20 to 1.54) |
b0.00001 |
89 |
|
18,847/95,149 |
20,925/301,713 |
0.05 (0.03 to 0.07) |
1.44 (1.28 to 1.63) |
b0.00001 |
92 |
|
|
18,144/93,604 |
20,842/301,525 |
0.05 (0.03 to 0.06) |
1.43 (1.26 to 1.62) |
b0.00001 |
92 |
|
|
733/1710 |
100/319 |
0.10 (0.05 to 0.16) |
1.55 (1.20 to 2.00) |
0.0009 |
0 |
|
|
1046/6627 |
1452/10,526 |
0.06 (0.00 to 0.12) |
1.43 (1.04 to 1.97) |
0.03 |
86 |
|
|
2272/6936 |
1061/3570 |
0.04 (0.00 to 0.08) |
1.11 (0.88 to 1.40) |
0.40 |
70 |
|
|
774/6277 |
922/6940 |
-0.02 (-0.08 to 0.04) |
0.92 (0.80 to 1.05) |
0.22 |
23 |
|
|
10,531/24419 |
2414/8020 |
0.10 (0.07 to 0.13) |
1.58 (1.43 to 1.74) |
b0.00001 |
45 |
|
|
Serious risk [47,49,50-53,58,59,66,67,51-53,56,58,59,66,67,69] |
7572/64,618 |
17,606/286,884 |
0.04 (0.03 to 0.05) |
1.70 (1.42 to 2.02) |
b0.00001 |
91 |
Table 3
Association between endotracheal tube intubation versus supraglottic airway (SGA) for survival to admission following cardiopulmonary resuscitation.
Group Events/total no of patients Risk difference, % (95%CI) Relative odds I2%
|
ETT |
SGA |
Odds ratio (95%CI) |
p value |
|||
|
11,730/33,561 |
5235/18,195 |
0.05 (0.02 to 0.09) |
1.36 (1.12 to 1.66) |
0.002 |
91 |
|
|
Analysis after duplicate database removal |
11,040/31878 |
3819/14473 |
0.05 (0.02 to 0.10) |
1.38 (1.10 to 1.72) |
0.005 |
92 |
|
11,657/33,234 |
5206/18,016 |
0.06 (0.02 to 0.10) |
1.41 (1.14 to 1.74) |
0.0001 |
93 |
|
|
Manual chest compressions [7,49,50,52,53,55,58,59,60,61,63,64,70,71] |
11,254/31,849 |
5190/17,876 |
0.05 (0.01 to 0.09) |
1.30 (1.06 to 1.61) |
0.01 |
92 |
|
476/1712 |
45/319 |
0.08 (-0.04 to 0.20) |
2.16 (1.54 to 3.02) |
b0.00001 |
0 |
|
|
1078/2711 |
1580/5103 |
0.04 (-0.02 to 0.10) |
1.23 (0.88 to 1.73) |
0.23 |
81 |
|
|
1346/5733 |
646/3181 |
0.03 (-0.03 to 0.08) |
1.26 (0.82 to 1.93) |
0.29 |
54 |
|
|
910/2207 |
1122/2745 |
-0.01 (-0.03 to 0.02) |
0.97 (0.86 to 1.09) |
0.59 |
0% |
|
|
8895/24915 |
1932/8143 |
0.09 (0.04 to 0.14) |
1.61 (1.24 to 2.09) |
0.0003 |
89 |
|
|
1925/6439 |
2181/7307 |
0.05 (0.00 to 0.09) |
1.30 (1.01 to 1.68) |
0.04 |
75 |
analyses. This only serves to illustrate the complexity of post arrest neu- rological outcomes, beyond simply avoiding hypoxia. Even in the most well designed RCT it would be difficult to control for key intra arrest var- iables (e.g. cause of arrest [78], antiarrhythmic used [79]) or post arrest care (e.g. cooling [80], blood pressure management [73]).
Limitations
The predominant limitation to this review is the lack of RCTs and a significant number of retrospective studies from overlapping databases. On the subgroup analysis removing the overlapping studies, this did not affect any of the results. This inconsistency of reported outcomes has been highlighted in Critical care literature remains a significant limita- tion to the conclusions drawn from the present study. Furthermore, the five RCTs utilized different Supraglottic airways, which may impact the overall outcome.
The diminishing effect of the overall result on longer term outcomes such as neurological status on discharge likely reflects the multifactorial nature of arrest cause, provider type and management strategy. The ma- jority of studies included in the present review do not control for or even mention many variables such as antiarrhythmic used and post ROSC management. This has a significant bearing on the conclusions drawn from the longer term outcomes included in the present study.
Conclusion
The present study showed a significant benefit with use of endotra- cheal intubation over supraglottic airway, however this is likely the re- sult of numerous other factors related to the cause and management of cardiac arrest. Five low risk studies provide a generalised level one rec- ommendation that overall there is no benefit for endotracheal intuba- tion over supraglottic airway devices. In the situation of automated
Association between endotracheal tube (ETT) intubation versus supraglottic airway (SGA) for survival to discharge following cardiopulmonary resuscitation.
|
Group |
Events/total no |
of patients |
Risk difference, % (95%CI) |
Relative odds |
I2% |
|
|
ETT |
SGA |
Odds ratio (95%CI) |
p value |
|||
|
7826/120,274 |
13,898/320,290 |
0.01 (0.00 to 0.02) |
1.28 (1.02 to 1.60) |
0.03 |
96 |
|
|
Analysis after duplicate database removal [6,7,47,50-58,60,61,63,65,70-72] |
7171/105599 |
12,474/286928 |
0.01 (0.00 to 0.03) |
1.33 (1.02 to 1.72) |
0.03 |
97 |
|
7826/120,274 |
13,898/320,290 |
0.01 (0.00 to 0.02) |
1.28 (1.02 to 1.60) |
0.03 |
96 |
|
|
Manual chest compressions [6,7,14,47,50-56,58,60,61,63,65-67,70-72] |
7712/118646 |
13,882/320013 |
0.01 (0.00 to 0.02) |
1.28 (1.02 to 1.61) |
0.04 |
96 |
|
Automated chest compressions |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
595/6794 |
682/10859 |
0.03 (0.01 to 0.06) |
1.80 (1.14 to 2.83) |
0.01 |
85 |
|
|
528/7810 |
564/3574 |
-0.02 (-0.14 to 0.09) |
0.96 (0.32 to 2.90) |
0.94 |
97 |
|
|
512/6111 |
593/6792 |
-0.01 (-0.03 to 0.02) |
0.90 (0.68 to 1.20) |
0.49 |
70 |
|
|
4243/48513 |
1917/31352 |
0.03 (0.01 to 0.05) |
1.54 (1.11 to 2.15) |
0.01 |
92 |
|
|
3071/65,650 |
11,388/282,146 |
0.00 (-0.01 to 0.02) |
1.34 (0.90 to 2.00) |
0.15 |
97 |
L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306 2305
Table 5
Association between endotracheal tube (ETT) intubation versus supraglottic airway (SGA) for survival to discharge with a neurologically intact state following cardiopulmonary resuscitation.
Group Events/total no of patients Risk difference, % (95%CI) Relative odds I2%
|
ETT |
SGA |
Odds ratio (95%CI) |
p value |
|||
|
3853/121,006 |
4579/317,255 |
0.01 (0.00 to 0.01) |
1.16 (0.94 to 1.41) |
0.16 |
91 |
|
|
Analysis after duplicate database removal [6,7,51,56,59,61,65,68,70,72] |
3628/106173 |
4130/283415 |
0.01 (0.00 to 0.02) |
1.17 (0.92 to 1.49) |
0.20 |
93 |
|
3853/121,006 |
4579/317,255 |
0.01 (0.00 to 0.01) |
1.16 (0.94 to 1.41) |
0.16 |
91 |
|
|
Manual chest compressions [6,7,47,51,56,58,59,61,63,65,67,68,70,72] |
3773/119378 |
4569/316,978 |
0.01 (0.00 to 0.01) |
1.15 (0.93 to 1.41) |
0.20 |
91 |
|
Automated chest compressions |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
356/5948 |
397/7981 |
0.01 (0.00 to 0.01) |
1.13 (0.95 to 1.33) |
0.17 |
13 |
|
|
162/2288 |
131/1904 |
0.01 (-0.06 to 0.08) |
1.14 (0.41 to 3.17) |
0.80 |
93 |
|
|
375/5902 |
418/6382 |
-0.01 (-0.03 to 0.02) |
0.88 (0.57 to 1.35) |
0.55 |
84 |
|
|
2313/47,076 |
744/30,782 |
0.02 (-0.01 to 0.05) |
1.46 (0.88 to 2.42) |
0.15 |
96 |
|
|
1165/68,028 |
3417/280,091 |
0.00 (0.00 to 0.00) |
1.06 (0.92 to 1.22) |
0.41 |
51 |
chest compressions endotracheal intubation will likely result in an early survival benefit.
Conflict of interest
The authors have no conflicts of interest to declare.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi. org/10.1016/j.ajem.2018.09.045.
References
- Graham R, McCoy MA, Schultz AM, editors. Strategies to improve cardiac arrest sur- vival: a time to act. Washington (DC): National Academies Press; 2015.
- Callaway CW, Soar J, Aibiki M, et al, Advanced Life Support Chapter Collaborators. Part 4: advanced life support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recom- mendations. Circulation 2015;132(16 suppl. 1):S84-S145.
- Wang HE, Simeone SJ, Weaver MD, et al. Interruptions in cardiopulmonary resusci- tation from paramedic endotracheal intubation. Ann Emerg Med 2009;54:645-652. e1 [2].
- Wang HE, Lave JR, Sirio CA, et al. Paramedic intubation errors: isolated events or symptoms of larger problems? Health Aff 2006;25:501-9.
- Benoit JL, Gerecht RB, Steuerwald MT, McMullan JT. Endotracheal intubation versus supraglottic airway placement in out-of-hospital cardiac arrest: a meta-analysis. Re- suscitation 2015;93:20-6.
- Fukuda T, Ohashi-Fukuda N, Kondo Y, Hayashida K, Sekiguchi H, Kukita I. Endotra- cheal intubation versus supraglottic airway insertion after out-of-hospital cardiac arrest: a nationwide population-based cohort study. D94. Critical care: translating practice to outcomes for our patients with acute critical illness. American Thoracic Society; 2018. p. A7378.
- Bernhard M, Behrens NH, Wnent J, Seewald S, Brenner S, Jantzen T, et al. Out-of-hos- pital airway management during Manual compression or automated chest compres- sion devices. Anaesthesist 2018:1-9.
- Jabre P, Penaloza A, Pinero D, Duchateau FX, Borron SW, Javaudin F, et al. Effect of Bag-mask ventilation vs endotracheal intubation during cardiopulmonary resuscita- tion on neurological outcome after out-of-hospital cardiorespiratory arrest: a ran- domized clinical trial. JAMA 2018;319(8):779-87.
- Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
- Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interven- tions. BMJ 2016;355:i4919.
- Puhan MA, Schunemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE Working Group approach for rating the quality of treatment effect esti- mates from Network meta-analysis. BMJ 2014;349:g5630.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta- analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283(15):2008-12.
- Abo BN, Hostler D, Wang HE. Does the type of out-of-hospital airway interfere with other cardiopulmonary resuscitation tasks? Resuscitation 2007;72(2):234-9.
- Benger J, Coates D, Davies S, Greenwood R, Nolan J, Rhys M, et al. Randomised com- parison of the effectiveness of the laryngeal mask airway supreme, i-gel and current practice in the initial airway management of out of hospital cardiac arrest: a feasibil- ity study. Br J Anaesth 2016;116(2):262-8.
- Deakin CD, Clarke T, Nolan J, Zideman DA, Gwinnutt C, Moore F, et al. A critical reas- sessment of ambulance service airway management in prehospital care: Joint Royal
Colleges Ambulance Liaison Committee Airway Working Group, June 2008. Emerg Med J 2010;27(3):226-33.
Edwards T, Williams J, Cottee M. Influence of prehospital airway management on neurological outcome in patients transferred to a heart attack centre following out-of-hospital cardiac arrest. Emerg Med Australas 2018.
- Fukuda T, Fukuda-Ohashi N, Doi K, Matsubara T, Yahagi N. Effective pre-hospital care for out-of-hospital cardiac arrest caused by respiratory disease. Heart Lung Circ 2015;24(3):241-9.
- Fullerton JN, Roberts KJ, Wyse M. Can experienced paramedics perform tracheal in- tubation at cardiac arrests? Five years experience of a regional Air ambulance service in the UK. Resuscitation 2009;80(12):1342-5.
- Gahan K, Studnek JR, Vandeventer S. King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resusci- tation 2011;82(12):1525-8.
- Guyette FX, Wang H, Cole JS. King airway use by air medical providers. Prehosp Emerg Care 2007;11(4):473-6.
- Hagihara A, Onozuka D, Nagata T, Hasegawa M. Effects of advanced life support on patients who suffered cardiac arrest outside of hospital and were defibrillated. Am J Emerg Med 2018;36(1):73-8.
- Hansen M, Lambert W, Guise JM, Warden CR, Mann NC, Wang H. Out-of-hospital pe- diatric airway management in the United States. Resuscitation 2015;90:104-10.
- Hillis M, Sinclair D, Butler G, Cain E. Prehospital Cardiac arrest survival and neuro- logic recovery. J Emerg Med 1993;11(3):245-52.
- Hilton MT, Wayne M, Martin-Gill C. Impact of system-wide king LT airway imple- mentation on orotracheal intubation. Prehosp Emerg Care 2016;20(5):570-7.
- Hiltunen P, Jantti H, Silfvast T, Kuisma M, Kurola J. Airway management in out-of- hospital cardiac arrest in Finland: current practices and outcomes. Scand J Trauma Resusc Emerg Med 2016;24(1):49.
- Kempema J, Ali S, Cabanas JG, Hinchey PR, Brown LH, Brown CV. Prehospital endo- tracheal intubation vs extraglottic airway device in blunt trauma. Am J Emerg Med 2015;33(8):1080-3.
- Kim YT, Do Shin S, Hong SO, Ahn KO, Ro YS, Song KJ, et al. Effect of national imple- mentation of utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from Out-of-Hospital cardiac arrest: a ten-year observa- tional study in Korea. BMJ Open 2017;7(8):e016925.
- Kurz MC, Prince DK, Christenson J, Carlson J, Stub D, Cheskes S, et al. Association of advanced airway device with chest compression fraction during out-of-hospital car- diopulmonary arrest. Resuscitation 2016;98:35-40.
- Middleton PM, Simpson PM, Thomas RE, Bendall JC. Higher insertion success with the i-gel(R) supraglottic airway in out-of-hospital cardiac arrest: a randomised con- trolled trial. Resuscitation 2014;85(7):893-7.
- Muller JU, Semmel T, Stepan R, Seyfried TF, Popov AF, Graf BM, et al. The use of the laryngeal tube disposable by paramedics during out-of-hospital cardiac arrest: a prospectively observational study (2008-2012). Emerg Med J 2013;30(12):1012 [emermed-2012].
- Nagao T, Kinoshita K, Sakurai A, Yamaguchi J, Furukawa M, Utagawa A, et al. Effects of bag-mask versus advanced airway ventilation for patients undergoing prolonged cardiopulmonary resuscitation in pre-hospital setting. J Emerg Med 2012;42(2): 162-70.
- Naito H, Yumoto T, Maeyama H, Tsukahara K, Okazaki Y, Mikane T, et al. Two differ- ent medical direction for airway management in a single city did not affect outcome of out-of-hospital cardiac arrest patients; 2017.
- Nakahara S, Tomio J, Ichikawa M, Morimura N, Nishida M, Sakamoto T. Effectiveness of advanced airway management by paramedics for witnessed out-of-hospital car- diac arrest of Cardiac origin. Resuscitation 2010;81(2):S18.
- Ohashi-Fukuda N, Fukuda T, Yahagi N. Effect of pre-hospital advanced airway man- agement for out-of-hospital cardiac arrest caused by respiratory disease: a propen- sity score-matched study. Anaesth Intensive Care 2017;45(3).
- Ono Y, Hayakawa M, Maekawa K, Mizugaki A, Katabami K, Wada T, et al. Should la- ryngeal tubes or masks be used for out-of-hospital cardiac arrest patients? Am J Emerg Med 2015;33(10):1360-3.
- Pakkanen T, Virkkunen I, Silfvast T, Randell T, Huhtala H, Ylli-Hankala A. One- year outcome after prehospital intubation. Acta Anaesthesiol Scand 2015;59 (4):524-30.
2306 L. White et al. / American Journal of Emergency Medicine 36 (2018) 2298-2306
Raatiniemi L, Lankimaki S, Martikainen M. pre-hospital airway management by non- physicians in northern Finland-a cross-sectional survey. Acta Anaesthesiol Scand 2013;57(5):654-9.
- Rehn M, Hyldmo PK, Magnusson V, Kurola J, Kongstad P, Rognas L, et al. Scandina- vian SSAI clinical practice guideline on pre-hospital airway management. Acta Anaesthesiol Scand 2016;60(7):852-64.
- Sanghavi P, Jena AB, Newhouse JP, Zaslavsky AM. Outcomes after out-of-hospital cardiac arrest treated by basic vs advanced life support. JAMA Intern Med 2015; 175(2):196-204.
- Sollid SJ, Bredmose PP, Nakstad AR, Sandberg M. A prospective survey of critical care procedures performed by physicians in helicopter emergency medical service: is clinical exposure enough to stay proficient? Scand J Trauma Resusc Emerg Med 2015;23(1):45.
- Sunde GA, Heltne JK, Lockey D, Burns B, Sandberg M, Fredriksen K, et al. Airway management by physician-staffed helicopter emergency medical services-a pro- spective, multicentre, observational study of 2,327 patients. Scand J Trauma Resusc Emerg Med 2015;23(1):57.
- Takyu H, Tanaka H, Nakagawa T. Does the airway management device for out-of- hospital cardiac arrest have no effect to patient’s outcome?; 2014.
- Vezina MC, Trepanier CA, Nicole PC, Lessard MR. Complications associated with the esophageal-tracheal Combitube(R) in the pre-hospital setting. Can J Anesth 2007;54 (2):124.
- Voss S, Rhys M, Coates D, Greenwood R, Nolan JP, Thomas M, et al. How do para- medics manage the airway during out of hospital cardiac arrest? Resuscitation 2014;85(12):1662-6.
- Wang HE, Kupas DF, Paris PM, Bates RR, Yealy DM. Preliminary experience with a prospective, multi-centered evaluation of Out-of-hospital endotracheal intubation. Resuscitation 2003;58(1):49-58.
- Wang HE, Mann NC, Mears G, Jacobson K, Yealy DM. Out-of-hospital airway man- agement in the United States. Resuscitation 2011;82(4):378-85.
- Yanagawa Y, Sakamoto T. Analysis of prehospital care for cardiac arrest in an urban setting in Japan. J Emerg Med 2010;38(3):340-5.
- Zhang JG, Fu WL, Qian LN, Lu ML, Zhang M. Evaluation of the effect of a clinical path- way on the quality of simulated pre-hospital cardiopulmonary resuscitation: pri- mary experience from a Chinese pre-hospital care centre. Hong Kong Eur J Emerg Med 2015;22(1):14-22.
- Becker TK, Berning AW, Prabhu A, Callaway CW, Guyette FX, Martin-Gill C. An as- sessment of ventilation and perfusion markers in out-of-hospital cardiac arrest pa- tients receiving mechanical CPR with endotracheal or supraglottic airways. Resuscitation 2018;122:61-4.
- Cady CE, Weaver MD, Pirrallo RG, Wang HE. Effect of emergency medical technician-placed Combitubes on outcomes after out-of-hospital cardiopulmonary arrest. Prehosp Emerg Care 2009;13(4):495-9.
- Chiang WC, Hsieh MJ, Chu HL, Chen AY, Wen SY, Yang WS, et al. The effect of suc- cessful intubation on patient outcomes after out-of-hospital cardiac arrest in Taipei. Ann Emerg Med 2018;71(3):387-96.
- Davey P, Dicker B. Outcome comparison between endotracheal intubation and la- ryngeal mask airway use in out-of-hospital cardiac arrest: a New Zealand registry study. Heart Lung Circ 2016;25:S8.
- Do Shin S, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and Cardiac arrest outcomes: a propensity score matched analysis. Resuscitation 2012;83 (3):313-9.
- Evans CC, Petersen A, Meier EN, Buick JE, Schreiber M, Kannas D, et al. Prehospital traumatic cardiac arrest: management and outcomes from the resuscitation out- comes consortium epistry-trauma and PROPHET registries. J Trauma Acute Care Surg 2016;81(2):285.
- Arslan Hanif M, Kaji AH, Niemann JT. Advanced airway management does not im- prove outcome of out-of-hospital cardiac arrest. Acad Emerg Med 2010;17(9): 926-31.
- Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced air- way management with neurologic outcome and survival in patients with out-of- hospital cardiac arrest. JAMA 2013;309(3):257-66.
- Jarman AF, Hopkins CL, Hansen JN, Brown JR, Burk C, Youngquist ST. Advanced air- way type and its association with chest compression interruptions during out-of- hospital cardiac arrest resuscitation attempts. Prehosp Emerg Care 2017;21(5): 628-35.
- Kajino K, Iwami T, Kitamura T, Daya M, Ong MEH, Nishiuchi T, et al. Comparison of supraglottic airway versus endotracheal intubation for the pre-hospital treatment of out-of-hospital cardiac arrest. Crit Care 2011;15(5):R236.
- Kang K, Kim T, Ro YS, Kim YJ, Song KJ, Do Shin S. Prehospital endotracheal intubation and survival after out-of-hospital cardiac arrest: results from the Korean nationwide registry. Am J Emerg Med 2016;34(2):128-32.
- Lin SC, Hsu SC, Weng YM, Kuo CI, Cheng CW. Dose pre-hospital laryngeal mask air- way use has a survival benefit in non-shockable cardiac arrest? Signa Vitae: J Intesive Care Emerg Med 2013;9(1):1-6.
- McMullan J, Gerecht R, Bonomo J, Robb R, McNally B, Donnelly J, et al. Airway man- agement and out-of-hospital cardiac arrest outcome in the CARES registry. Resusci- tation 2014;85(5):617-22.
- Mulder PJ, Oetomo SB, Vloet L, de Vries P, Hoogerwerf N. Comparison in effective- ness and safety between a supraglottic airway device and endotracheal intubation in out-of-hospital cardiac arrest in the Netherlands. Resuscitation 2013;84:S17.
- Noda E, Zaitsu A, Hashizume M, Takahashi S. Prognosis of patient with cardiopulmo- nary arrest transported to Kyushu University Hospital. Fukuoka Igaku Zasshi 2007; 98(3):73-81.
- Rabitsch W, Schellongowski P, Staudinger T, Hofbauer R, Dufek V, Eder B, et al. Com- parison of a conventional tracheal airway with the combitube in an urban emer- gency medical services system run by physicians. Resuscitation 2003;57(1):27-32.
- Sulzgruber P, Datler P, Sterz F, Poppe M, Lobmeyr E, Keferbock M, et al. The impact of airway strategy on the patient outcome after out-of-hospital cardiac arrest: a pro- pensity score matched analysis. Eur Heart J Acute Cardiovasc Care 2017;7(5): 423-31 [2048872617731894].
- Takei Y, Enami M, Yachida T, Ohta K, Inaba H. Tracheal intubation by paramedics under limited indication criteria may improve the Short-term outcome of out-of- hospital cardiac arrests with noncardiac origin. J Anesth 2010;24(5):716-25.
- Tanabe S, Ogawa T, Akahane M, Koike S, Horiguchi H, Yasunaga H, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J Emerg Med 2013;44(2):389-97.
- Wang HE, Szydlo D, Stouffer JA, Lin S, Carlson JN, Vaillancourt C, et al. Endotracheal intubation versus supraglottic airway insertion in out-of-hospital cardiac arrest. Re- suscitation 2012;83(9):1061-6.
- Yeung J, Chilwan M, Field R, Davies R, Gao F, Perkins GD. The impact of airway man- agement on Quality of cardiopulmonary resuscitation: an observational study in pa- tients during cardiac arrest. Resuscitation 2014;85(7):898-904.
- Benger JR, Kirby K, Black S, Brett SJ, Clout M, Lazaroo MJ, et al. Effect of a strategy of a supraglottic airway device vs tracheal intubation during out-of-hospital cardiac ar- rest on functional outcome: the AIRWAYS-2 randomized clinical trial. JAMA Aug 28 2018;320(8):779-91.
- Erath JW, Buettner S, Weiler H, Vamos M, Von Jeinsen B, Heyl S, et al. P2733 prog- nostic implications of preclinical airway management with laryngeal tube (LTS-D) or endotracheal tube in out-of-hospital cardiac arrest patients. Eur Heart J Aug 1 2018(39(suppl_1)) [ehy565-P2733].
- Wang HE, Schmicker RH, Daya MR, Stephens SW, Idris AH, Carlson JN, et al. Effect of a strategy of initial laryngeal tube insertion vs endotracheal intubation on 72-hour survival in adults with out-of-hospital cardiac arrest: a randomized clinical trial. JAMA Aug 28 2018;320(8):769-78.
- Sunde K, Pytte M, Jacobsen D, Mangschau A, Jensen LP, Smedsrud C, et al. Implemen- tation of a standardised treatment protocol for post resuscitation care after out-of- hospital cardiac arrest. Resuscitation Apr 1 2007;73(1):29-39.
- Ong ME, Ornato JP, Edwards DP, Dhindsa HS, Best AM, Ines CS, et al. Use of an auto- mated, load-distributing band chest compression device for out-of-hospital cardiac arrest resuscitation. JAMA Jun 14 2006;295(22):2629-37.
- Safar P, Brown TC, Holtey WH, Wilder R. Ventilation and circulation with closed chest cardiac massage in man. JAMA 1961;176:574-6.
- Rottenberg EM. Overcoming the difficulties of bougie-assisted endotracheal intuba- tion. Am J Emerg Med Jan 2016;34(1):111-2.
- Pirotte M, Pirotte A, Trueger NS. Two cases of digitally assisted bougie intubation: a novel technique for difficult airway management. Am J Emerg Med 2015. https:// doi.org/10.1016/j.ajem.2015.04.052 [pii: S0735-6757(15)00319-8].
- Meyer L, Stubbs B, Fahrenbruch C, Maeda C, Harmon K, Eisenberg M, et al. Incidence, etiology, and survival trends from cardiovascular-related sudden cardiac arrest in children and young adults ages 0-35: a 30-year review. Circulation Jan 1 2012;126 (11):1325-7 [CIRCULATIONAHA-111].
- Chowdhury A, Fernandes B, Melhuish TM, White LD. Antiarrhythmics in cardiac arrest: a systematic review and meta-analysis. Heart Lung Circ Aug 23 2017;122(2):e115.
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to im- prove the neurologic outcome after cardiac arrest. N Engl J Med 2002;346(8): 549-56.
