Comparing intranasal ketamine with intravenous fentanyl in reducing pain in patients with renal colic: A double-blind randomized clinical trial
a b s t r a c t
Background: Kidney stones are a fairly common problem that manifests itself as symptoms of acute abdominal and flank pains in patients presenting to emergency departments.
Objective: The present study was conducted to compare the analgesic effect of intravenous fentanyl with that of
intranasal ketamine in renal colic patients.
Methods: One mg/kg of intranasal ketamine was administered in the first group, and one ug/kg of intravenous fentanyl in the second group. The Pain severity was measured in the patients in terms of a Visual Analogue Scale score at the beginning of the study and at minutes 5, 15 and 30, and the medication side-effects were evaluated and recorded.
Results: A total of 130 patients were ultimately assessed in two groups of 65. In the ketamine group, the mean severity of pain was 8.72 +- 1.52 at the beginning of the study (P b 0.001), 5.5 +- 2.97 at minute 5 (P b 0.001),
3.38 +- 3.35 at minute 15 (P = 0.004) and 2.53 +- 3.41 at minute 30 (P = 0.449). In the fentanyl group, this se- verity was 9.66 +- 88.8 in the beginning of the study (P b 0.001), 7.27 +- 1.37 at minute 5 (P b 0.001), 4.61 +- 1.5 at minute 15 (P = 0.004) and 1.24 +- 1.25 at minute 30 (P = 0.449). The general prevalence of the medication side- effects was 10 (15.4%) in the ketamine group and 1 (1.5%) in the fentanyl group (P = 0.009). Conclusions: Ketamine was found to be less effective than fentanyl in controlling renal colic-induced pain, and to be associated with a higher prevalence of side-effects; nevertheless, ketamine can be effective in controlling this pain in conjunction with other medications.
(C) 2019
Introduction
Kidney stones are a fairly common problem that manifests itself as symptoms of acute abdominal and flank pains in patients presenting to emergency departments [1]. These patients account for approxi- mately 1% of presentations to emergency departments [2]. The regis- tered prevalence of kidney stones is 1%-5% in Asia, 5%-9% in Europe and 13% in America [3]. Renal colic affects 5%-15% of the world’s popu- lation [4]. In industrial communities, 5%-12% of people generally expe- rience renal colic at least once in their life, about 50% of whom experience recurrence, and those with a positive family history are three times more at risk for developing kidney stones [5].
Patient pain is normally managed using intravenous analgesics in emergency departments [6,7]. Renal colic is mainly treated to reduce the frequency of administrating analgesics. The two commonly-used medication groups, with many contraindications and side-effects though [8], include injectable NSAIDs and opiates in case of failing to re- spond to the treatment [8,9].
E-mail address: [email protected] (M. Maleki Verki).
Although NSAIDs cause fewer frequencies of nausea, vomiting, respi- ratory suppression and drowsiness compared to opiates, they cause po- tential side-effects, including platelet dysfunction, nephropathy and increased cardiovascular mortality in IHD. Given the numerous side- effects of NSAIDs and opiates, discovering new medications with fewer side-effects and adequate analgesic properties appears essential [10].
Fentanyl is a strong derivative of phenylpiperidine, and its effects in- clude mitigation of pain, euphoria and relief, respiratory and cough sup- pression, nausea and vomiting, pupil constriction, reduced bowel movements and histamine release with the subsequent bronchial con- traction and hypotension. Its most common unwanted complications include constipation and hypotension. It is rapid-acting with short pe- riods of effect, and is especially used to control acute pains [11,12]. Ke- tamine is used as a general anesthetic in short surgeries or Diagnostic procedures requiring no musculoskeletal relaxation. Ketamine probably exerts its effects by inhibiting neurological pain signals and reducing spinal activities. In very special cases, the contraindications of ketamine include severe cardiovascular diseases, Severe hypertension, recent myocardial infarction, heart attack and brain traumas [13,14]. Given its profound Analgesic effects and minimum respiratory depression,
https://doi.org/10.1016/j.ajem.2019.05.049
0735-6757/(C) 2019
this medicine causes few predictable complications, and is mostly ad- ministered intravenously or intramuscularly [15].
As opposed to the intravenous way, this medicine can also be admin- istered through the intranasal way. Research suggests that intranasal ketamine is a popular medicine used in this way. Intranasal ketamine is an effective analgesic with minimal effects on the heart [16]. The pres- ent study was conducted to investigate the effectiveness of intranasal ketamine, as an alternative method with fewer complications, in allevi- ating pain in patients with renal colic.
Materials and methods
Trial design and participants
This study was conducted according to the Consolidated Standards of Reporting Trials (CONSORT) [17]. The present double-blind clinical trial was conducted in 2017-18 to compared intranasal ketamine and intravenous fentanyl in terms of pain relief in patients with kidney stone-induced pain presenting to the emergency department of Ahvaz Golestan and Imam Khomeini Hospitals. After receiving the permission of the Ethics Committee of IR.AJUMS.REC.1397.019 University of Medi- cal Sciences and a code for the clinical trial, the present study was con- ducted based on the ethical principles regarding human experimentation stipulated in the Declaration of Helsinki.
The eligible candidates included all 15-65 year-old patients with typical kidney stone symptoms presenting to the hospital, patients with no history of kidney stones confirmed through CT scan and ultra- sound, those who were willing to participate in the study, patients with radiating symptoms to genitalia, nausea, vomiting, urinary irrita- tion and costovertebral angle tenderness.
The exclusion criteria comprised Opioid dependence, a history of psychological disorders in the patients or their first-degree relatives, fluctuations in alertness, receiving analgesics up to 6 h before entering the emergency department, unconfirmed renal colic caused by kidney stones, withdrawal from the study at any point, a history of seizure, chronic renal disease, Chronic liver disease, chronic respiratory diseases, metabolic diseases, brain tumors, pregnancy, cardiovascular diseases and glaucoma, being younger than 15 or older than 65 years old, speech disability, a history of sensitivity to ketamine or fentanyl, cerebral ab- normality, SBP N 180 or SBP b 90, hydrocephaly, breastfeeding, respira- tory distress, nasal obstruction, abdominal tenderness suspected of peritonitis, head traumas and a body temperature of over 38 ?C.
Intervention
Simple random sampling was used to select the patients and ran- domly assign them to the ketamine and fentanyl groups. Every patient was given a block randomization code, and assigned to a specific group, of which only the main researcher and the triage nurse were aware. A specific medication was prepared and its dose determined by the triage nurse based on the patient’s code, and administered by the emergency physician, who was unaware of the study protocol. The first group re- ceived 1 mg/kg of intranasal drops of ketamine and a volume of IV dis- tilled water equal to fentanyl proportional to the patient’s weight, and the second group received 1 ug/(kg/bw) IV fentanyl from a 50 ug/ml solu- tion and intranasal drops of distilled water equal in volume to ketamine proportional to the patient’s weight in a double-blind fashion. Before be- ginning the study, the patients were briefed on the medication adminis- tration method and side-effects. The patients were monitored by the emergency physician while receiving the treatment.
Outcomes
In the beginning of the study, the patients were asked to determine their degree of pain using a VAS on a range of zero denoting no pain to 10 denoting the worst pain. Vital signs, nausea, vomiting, dysuria,
hematuria and other parameters were recorded. Moreover, the patients’ severity of pain and possible side-effects were evaluated and recorded 5, 15 and 30 min after the medication administration.
The study ended when every patient received a VAS score of below 3 for 30 min after receiving the last analgesic or one of the cited medi- cines. The patients with a VAS score of over 3 received 0.1 mg/kg of IV morphine as the rescue analgesic. Liquid-therapy was not routinely ad- ministered in the present study unless the patients were dehydrated or developed sepsis. The patients received a total of 10 ml/kg of liquid. Side-effects including nausea, vomiting, hematuria, dysuria, headache, dizziness and agitation were recorded in the patients. Furthermore, vital signs including systolic and diastolic blood pressures, heart rate and respiratory rate were regularly measured during the study so as to record variations in hypotension and bradycardia in the patients.
Statistical analysis
After collecting and initially processing the data, the observations were recorded, described and analyzed in SPSS. All the observations were first described using descriptive statistics, including frequency ta- bles, frequency distribution diagrams and column charts and statistical measures of central tendency and dispersion. The Kolmogorov- Smirnov test was used to investigate the Study objectives and hypothe- ses as well as the distribution normality of the data. The t-test was used to investigate the relationship among the normally-distributed quanti- tative variables, and the Mann-Whitney U test among the non-normal data. The Chi-square and Fisher’s exact tests were also used to evaluate the relationship among the qualitative variables. P b 0.05 was set as the level of statistical significance.
Results
Baseline data
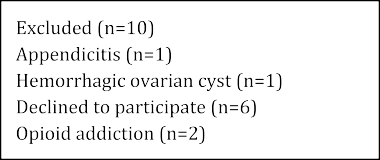
A total of 130 patients, including 40 (30.8%) females, were investi- gated in two groups of 65 (Fig. 1). The mean age of the participants was 36.93 +- 10.55 years. The participants weighed 50-125 kg and had a mean weight of 75.03 +- 13.46 kg.
Findings
The mean degree of pain was found to be significantly higher in the fentanyl group compared to in the ketamine group in the beginning of the study and at the 5th and 15th minutes. This mean was, however, higher in the ketamine group at the 30th minute, although no signifi- cant differences were observed at this stage between the two groups (P = 0.449) (Fig. 2). A significant declining trend was also observed in the pain severity in both groups from the beginning of the study to the 5th, 15th and 30th minutes (P b 0.001).
The mean heart rate was significantly higher in the fentanyl group compared to in the ketamine group in the beginning of the study and at the 5th, 15th and 30th minutes (P b 0.001). Respiratory rate was also sig- nificantly higher in the fentanyl group compared to in the ketamine group in the beginning of the study (P b 0.001) and at the 5th minute (P = 0.001), although no significant differences were observed between the two groups at the 15th minute (P = 0.616), while it was significantly higher in the ketamine group at the 30th minute (P b 0.001). The mean arterial systolic blood pressure was significantly higher in the fentanyl group compared to in the ketamine group in the beginning of the study (P b 0.001), although no significant differences were observed between the two groups at the 5th minute (P = 0.64), while it was significantly higher in the ketamine group compared to in the fentanyl group at the 15th (P = 0.025) and 30th minutes (P = 0.003). No significant differ- ences were, however, observed between the two groups in the mean di- astolic blood pressure at any time points (P N 0.05).



















The overall prevalence of the medication-induced side-effects was found to be 10 (15.4%) in the ketamine group and 1 (1.5%) in the fenta- nyl group, suggesting significant differences between the two groups (P
= 0.009). The most common side-effects observed in both groups were
nausea and vomiting, although the prevalence of neither was signifi- cantly different between the two groups (Table 1). Thirty minutes after the administration of medication, additional analgesics were needed in 21 (32.3%) patients in the ketamine group and 6 (9.2%) in the fentanyl group (P = 0.002), suggesting a more effective pain control in the fentanyl group (P = 0.002).
Discussion
The present results showed that ketamine and fentanyl significantly alleviate the pain in the patients in the first 30 min following the med- ication administration (P b 0.001). The mean severity of pain was signif- icantly higher in the fentanyl group compared to in the ketamine group in the beginning of the study and at the 5th and 15th minutes. The dif- ference between the two groups reduced over time, and the severity of pain in the fentanyl group fell below that IN ketamine group at the 30th minute (P = 0.449). However a VAS of 2.5 and 1.5 between the different




Fig. 2. Pain score trend during the study follow up.
side effects after intervention.
|
Side effect |
Ketamine (N = 65) |
Fentanyl (N = 65) |
P-value |
|
Nausea |
13 (20%) |
9 (13.8%) |
0.484 |
|
Vomiting |
10 (15.4%) |
9 (13.8%) |
0.9 |
|
Headache |
3 (4.6%) |
1 (1.5%) |
0.619 |
|
Dizziness |
4 (6.2%) |
1 (1.5%) |
0.365 |
|
Agitation |
1 (1.5%) |
1 (1.5%) |
0.99 |
groups respectively is clinically relevant even though statistically the Fentanyl group was better. Furthermore, 30 min after the medication, 21 (32.3%) patients in the ketamine group and 6 (9.2%) in the fentanyl group needed additional analgesics (P = 0.002), which suggested a bet- ter pain control in the fentanyl group.
Few studies have so far been clinically conducted to investigate the effectiveness of intranasal ketamine in reducing pain in renal colic pa- tients. The majority of these studies have well identified and reported the analgesic effects of ketamine in emergency departments. In line with the present study, Farnia M et al. [18] compared the effect of intra- nasal ketamine with IV morphine in 2015 on reducing pain in patients with renal colic, and showed that the pain was significantly more severe in the ketamine group compared to in the morphine group in the begin- ning of the study and at minute 5, although they observed no significant differences between the two groups at the 15th and 30th minutes. In contrast to the present research, they reported lower needs for addi- tional analgesics in the ketamine group compared to in the morphine group, although the difference was statistically insignificant.
Shimonovich et al. [19] compared intranasal ketamine with IV and intramuscular morphine in terms of acute injury-induced pain, and re- ported that the analgesic effect and safety of ketamine are comparable to IV and intramuscular morphine; nevertheless, they recommended further research for confirming the analgesic effect of intranasal keta- mine in emergency departments.
Frouzan et al. [20] also compared intranasal ketamine with IV mor- phine in patients with orthopedic fractures, and found the severity of pain to be significantly lower in the morphine group compared to in the ketamine group. Moreover, they found morphine to exert its analge- sic effects fasters than ketamine in a way that the mean time of the emergence of pain was 5.09 min in the ketamine group and 2.36 min in the morphine group (P = 0.003).
In 2016, Shrestha et al. [21] showed that intranasal ketamine re- duced the VAS pain score by at least two degrees in 80% of the patients 15 min after the administration. Similarly, Yeaman et al. [22] found in- tranasal ketamine to be an appropriate analgesic in 56% of the patients, as it reduced the severity of pain by 2.4 units in terms of the VAS scale within 30 min. Moreover, Andolfatto et al. [7] found intranasal ketamine to reduce the pain score by at least 1.3 units in 88% of the cases, and ob- served a mean reduction of 3.4 in the VAS score in 30 min, which are consistent with the present study.
The Intranasal administration of medicines is considered a safe and ef- fective alternative path. Given that this method does not require setting up an IV route, it is more tolerable in patients, and reduces the risk of nee- dle stick in emergency situations, especially in uncooperative patients.
The overall prevalence of the medication-induced side-effects was 10 (15.4%) in the ketamine group and 1 (1.5%) in the fentanyl group (P = 0.009), all of which were mild and treated in the emergency de- partment. The most common side-effects observed in both groups were also nausea and vomiting, although the prevalence of neither was significantly different between the two groups.
The frequency of the types of ketamine side-effects has been differ-
ently reported in literature, including the study by Shrestha et al. [21], and nearly all the reported side-effects were mild and transient. These authors found dizziness to be the most prevalent side-effect observed in 88% of the patients followed by nausea in 41.2%, which was severe only in one patient, as well as headache, delusion, fatigue and sickness
each in 6% of the patients. Andolfatto et al. [7] observed minor and tran- sient side-effects for intranasal ketamine, including dizziness in 53% of the patients, unrealistic feelings in 35%, nausea in 10%, mood changes in 8% and auditory changes in 3%.
In 2017, Reynolds et al. [23] compared intranasal ketamine with in- tranasal fentanyl, and found the most prevalent side-effects of ketamine to include bad taste in the mouth (90.2%), dizziness (73.2%) and drows- iness (46.3%), and those of fentanyl to include drowsiness (36.3%), bad taste in the mouth (22%) and itchy nose (22%). In line with the present study, these authors found ketamine to be associated with more minor side-effects compared to fentanyl. In 2018, Frey et al. also compared the effects of intranasal ketamine with those of fentanyl, and observed more side-effects, all of which minor and transient, in the participants receiv- ing ketamine. Beaudoin et al. [24] found the administration of especially
0.3 mg/kg of ketamine to be associated with dysphoria and dizziness. In- vestigating the patients’ vital signs also showed that administrating fen- tanyl was associated with a relative reduction in the heart rate, respiratory rate and systolic and diastolic blood pressures, and this ef- fect was more significant on blood pressure; ketamine, however, exerted no significant effects on the patients’ vital signs.
Study limitations
The main limitation of the present study included a disproportional distribution of men and women in the intervention groups. Given that renal colic develops more frequently in young and middle-aged men, the reduced rate in the women was predictable in the groups.
Conclusion
The present results showed that the effect of 1 mg/kg of intranasal ketamine is less significant than that of 1 ug/kg of IV fentanyl on control- ling pain in renal colic. Administrating ketamine was also associated with a higher prevalence of side-effects, including nausea and vomiting, headache, dizziness and agitation; nevertheless, given the minimal ef- fects of intranasal ketamine on patients’ vital signs, it may be effective in controlling renal colic pain in conjunction with other medicines.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgment
The authors wish to acknowledge the support of the deputy of re- search affairs of the Ahvaz Jundishapur University of Medical Sciences and Semnan University of Medical Sciences as part of Alireza Sabouhi’s thesis under the research code U-97006.
Funding source, financial disclosures
Ahvaz Jundishapur University of Medical Sciences number: U- 97006.
IRCT clinical trial registry
(IRCT20180523039805N1), http://www.irct.ir.
Ethic code
(IR.AJUMS.REC.1397.019).
Contribute
A.F and A.D: conceived the original idea, designed the scenarios and collected the data.
S.Z and H.M: carried out the analysis of data, drafted the manuscript,
A.D: revised it, drafted the manuscript, approved the final version that was submitted.
References
- Ramos-Fernandez M, Serrano LA. Evaluation and management of renal colic in the emergency department. Bol Asoc Med P R 2009;101(3):29-32.
- Maleki Verki M, Porozan S, Motamed H, Fahimi MA, Aryan A. Comparison the anal- gesic effect of Magnesium sulphate and ketorolac in the treatment of renal colic pa- tients: double-blind clinical trial study. Am J Emerg Med 2019;37(6):1033-6.
- Cupisti A, Pasquali E, Lusso S, Carlino F, Orsitto E, Melandri R. Renal colic in Pisa emergency department: epidemiology, diagnostics and treatment patterns. Intern Emerg Med 2008;3(3):241-4.
- Walls R, Hockberger R, Gausche-Hill M. Rosen’s emergency medicine-concepts and clinical practice e-book. Elsevier Health Sciences; 2017.
- Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Ure- teral Stones Clinical Guidelines Panel summary report on the management of ure- teral calculi. The American Urological Association. J Urol 1997;158(5):1915-21.
- Leveridge M, D’Arcy FT, O’Kane D, Ischia JJ, Webb DR, Bolton DM, et al. Renal colic: current protocols for emergency presentations. Eur J Emerg Med 2016;23(1):2-7.
- Andolfatto G, Willman E, Joo D, Miller P, Wong WB, Koehn M, et al. Intranasal keta- mine for analgesia in the emergency department: a prospective observational series. Acad Emerg Med 2013;20(10):1050-4.
- Safdar B, Degutis LC, Landry K, Vedere SR, Moscovitz HC, D’Onofrio G. Intravenous morphine plus ketorolac is superior to either drug alone for treatment of acute renal colic. Ann Emerg Med 2006;48(2):173-81 [81 e1].
- Morteza-Bagi HR, Amjadi M, Mirzaii-Sousefidi R. The comparison of Apotel plus low dose of morphine and full dose of morphine in pain relief in patients with acute renal colic. Addict Health 2015;7(1-2):66-73.
- Masoumi K, Forouzan A, Asgari Darian A, Feli M, Barzegari H, Khavanin A. Compar- ison of clinical efficacy of intravenous acetaminophen with intravenous morphine in acute renal colic: a randomized, double-blind, controlled trial. Emerg Med Int 2014;2014:571326.
- Motamed H, Maleki Verki M. intravenous lidocaine compared to fentanyl in renal colic pain management; a randomized clinical trial. Emergency (Tehran, Iran) 2017;5(1):e82.
- Poklis A. Fentanyl: a review for clinical and analytical toxicologists. J Toxicol Clin Toxicol 1995;33(5):439-47.
- Laskowski K, Stirling A, McKay WP, Lim HJ. A systematic review of intravenous keta- mine for postoperative analgesia. Can J Anaesth 2011;58(10):911-23.
- Khademi S, Ghaffarpasand F, Heiran HR, Yavari MJ, Motazedian S, Dehghankhalili M. Intravenous and peritonsillar infiltration of ketamine for postoperative pain after adenotonsillectomy: a randomized placebo-controlled clinical trial. Med Princ Pract 2011;20(5):433-7.
- Marx J, Walls R, Hockberger R. Rosen’s emergency medicine-concepts and clinical practice e-book. Elsevier Health Sciences; 2013.
- Weinbroum AA. Non-opioid IV adjuvants in the perioperative period: pharmacolog- ical and clinical aspects of ketamine and gabapentinoids. Pharmacol Res 2012;65(4): 411-29.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8(1):18.
- Farnia MR, Jalali A, Vahidi E, Momeni M, Seyedhosseini J, Saeedi M. Comparison of intranasal ketamine versus IV morphine in reducing pain in patients with renal colic. Am J Emerg Med 2017;35(3):434-7.
- Shimonovich S, Gigi R, Shapira A, Sarig-Meth T, Nadav D, Rozenek M, et al. Intranasal ketamine for acute traumatic pain in the Emergency Department: a prospective, randomized clinical trial of efficacy and safety. BMC Emerg Med 2016;16(1):43.
- Forouzan A, Masoumi K, Motamed H, Mozaffari J, Gharibi S. Comparison of intranasal ketamine versus intravenous morphine in pain relief of patient with bone fracture. Int J Adv Biotechnol Res 2017;8(4):1636-43.
- Shrestha R, Pant S, Shrestha A, Batajoo KH, Thapa R, Vaidya S. Intranasal ketamine for the treatment of patients with acute pain in the emergency department. World J Emerg Med 2016;7(1):19-24.
- Yeaman F, Meek R, Egerton-Warburton D, Rosengarten P, Graudins A. Sub-dissocia- tive-dose intranasal ketamine for moderate to severe pain in adult emergency de- partment patients. Emerg Med Australas 2014;26(3):237-42.
- Reynolds SL, Bryant KK, Studnek JR, Hogg M, Dunn C, Templin MA, et al. Randomized controlled feasibility trial of intranasal ketamine compared to Intranasal fentanyl for analgesia in children with suspected extremity fractures. Acad Emerg Med 2017;24 (12):1430-40.
- Beaudoin FL, Lin C, Guan W, Merchant RC. low-dose ketamine improves pain relief in patients receiving Intravenous opioids for acute pain in the emergency depart- ment: results of a randomized, double-blind, clinical trial. Acad Emerg Med 2014; 21(11):1193-202.
