High risk and low prevalence diseases: Testicular torsion
a b s t r a c t
Introduction: Testicular torsion is a Serious condition that carries with it a high rate of morbidity. Objective: This review highlights the pearls and pitfalls of testicular torsion, including presentation, diagnosis, and management in the emergency department (ED) based on current evidence.
Discussion: Testicular torsion is a urological emergency that occurs with rotation of the testicle along its supporting ligaments leading to obstruction of vascular flow. A key risk factor is the presence of a bell-clapper deformity. The most common population affected includes children in a bimodal distribution with the most cases occurring in the first year of life and between 12 and 18 years, although cases do occur in adults. Acute, se- vere, unilateral scrotal pain is the most common presenting symptom. Nausea and vomiting are common, but the presence or absence of a cremasteric reflex is not a reliable indicator of disease. The TWIST score may assist with clinical decision making in patients presenting with acute testicular pain but should not be used in isolation. If torsion is suspected or confirmed, consultation with the urology specialist should not be delayed, as outcomes are time sensitive. Ultrasound can be used for diagnosis, but a normal ultrasound examination cannot exclude the diagnosis. Treatment includes emergent urology consultation for surgical exploration and detorsion, as well as symptomatic therapy in the ED. Manual detorsion can be attempted in the ED while awaiting transfer or consultation.
Conclusions: An understanding of testicular torsion can assist emergency clinicians in diagnosing and managing this disease.
Published by Elsevier Inc.
This article series addresses high risk and low prevalence diseases that are encountered in the emergency department (ED). Much of the primary literature evaluating these conditions is not emergency medi- cine focused. By their very nature, many of these Disease states and clin- ical presentations have little useful evidence available to guide the emergency clinician in diagnosis and management. The format of each article defines the disease or clinical presentation to be reviewed, pro- vides an overview of the extent of what we currently understand, and finally discusses pearls and pitfalls using a question-and-answer format. This article will discuss testicular torsion. This condition’s low preva- lence but high morbidity, as well as its variable atypical patient
E-mail addresses: [email protected] (A. Lacy), [email protected] (A. Smith), [email protected] (B. Long).
1 Present Address: 3551 Roger Brooke Dr. Fort Sam Houston, TX 78234.
presentations and challenging diagnosis, makes it a high risk and low prevalence disease.
-
- Definition
Testicular torsion is defined by twisting of the testicle along the spermatic cord, resulting in venous congestion and poor arterial inflow, ultimately leading to ischemia [1-4]. Because of the morbidity and potential risk of infertility, testicular torsion is a urological emergency. Torsion primarily occurs due to abnormal or absent fixation of testicle and the tunica vaginalis [1-7]. The tunica vaginalis contains the spermatic cord and normally adheres to the posterolateral part of the testicle. An absent or abnormal fixation can result in twisting of the tes- ticle along the spermatic cord, which reduces Venous outflow and causes vascular congestion of the testicle [4,8,9]. This results in the tes- ticle becoming swollen, tender, and erythematous, and with continued twisting, arterial flow is reduced, resulting in ischemia and even perma- nent damage with infertility [1-6]. Damage is predominantly due to is- chemia from cord rotation leading to decreased arterial flow to the
https://doi.org/10.1016/j.ajem.2023.01.031 0735-6757/Published by Elsevier Inc.
ED management.>testicle [1-6]. Ischemia most commonly occurs 4-8 h after the onset of torsion [2,10].
The condition can be divided into intravaginal and extravaginal torsion. Intravaginal torsion refers to an abnormality with the tunica vaginalis attachment, most commonly a high attachment referred to as the bell clapper deformity, which allows the spermatic cord to twist within the tunica vaginalis [1-3,11] (Fig. 1). Neonates may develop the extravaginal form where the tunica vaginalis is not adhered to the gubernaculum, and thus the tunica vaginalis and spermatic cord twist together. This may occur weeks to months before birth [1-3].
-
- Epidemiology and outcomes
Scrotal complaints are common and account for approximately 0.5% of ED visits. Approximately 15-25% of patients with testicular pain or scrotal complaints who present to the ED will have testicular torsion, though there are a variety of other conditions or mimics of torsion (dis- cussed later) [4,12,13]. Testicular torsion occurs in all age groups, but it most commonly occurs after birth and between 12 and 18 years of age. The incidence is estimated to be 1 in 4000 males below the age of 25 [2,14], and another study found an annual incidence of 3.8 per 100,000 males <18 years [15]. However, up to 14% of cases occur in adults [4]. Outcomes depend on the severity or degree of torsion and is- chemia, as well as the time to detorsion. Testicular salvage is higher in patients under 21 years (41% vs 70% in those older than 21 years), which is likely due to delay in presentation and greater degree of cord twisting in older patients [4,16].
- Discussion
- Presentation
Testicular torsion most commonly presents in a young male patient with sudden, unilateral, moderate or severe scrotal/testicular pain, dif- fuse testicular tenderness, and swelling, [1,2,4]. These signs and symp- toms most commonly occur several hours after minor trauma to the testicles or physical activity, though patients may also awake from sleep with severe pain or have sudden pain at rest [1-4,17]. Patients can also present with nausea, vomiting, and lower abdominal pain. The abdominal pain may not localize to the testicle or scrotum in some cases [2,3,8,17]. Symptoms may be intermittent and self- resolving. Examination typically reveals an asymmetric high-riding
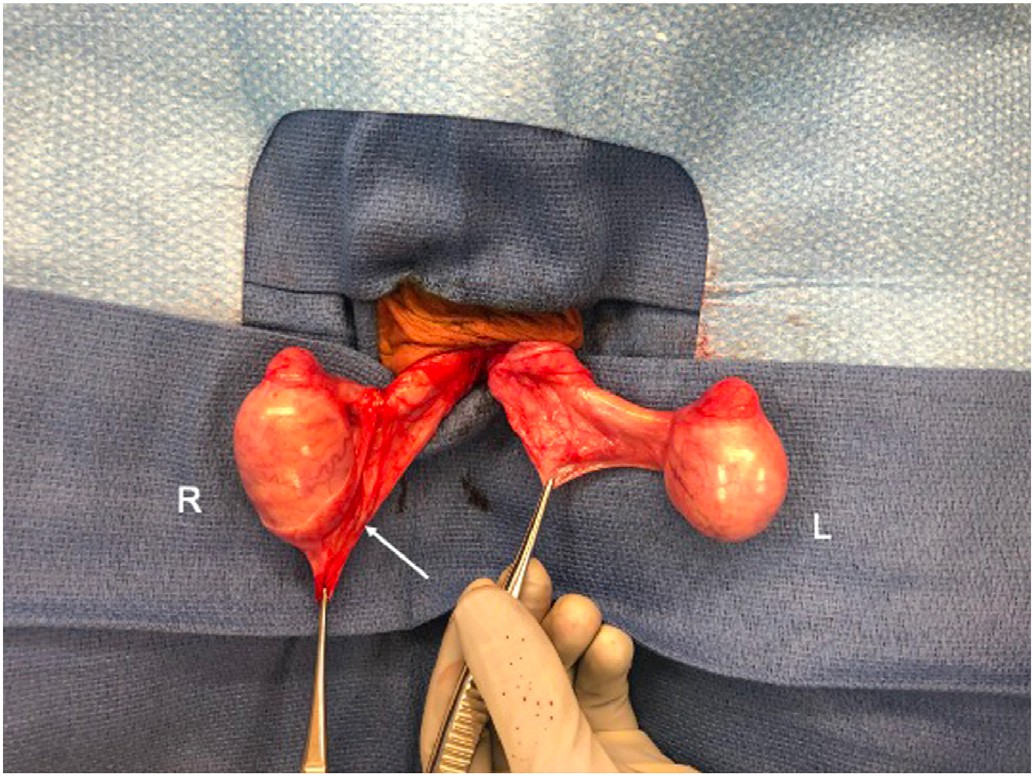
Fig. 1. Comparison of normal gubernacular attachment (white arrow) on the right testicle to the abnormal bell-clapper attachment of the left testicle leading to testicular torsion. Obtained with permission from Dr. Evalynn Vasquez [11].
testicle oriented with its long axis oriented transversely [3,4,8,17]. A twist in the spermatic cord may be palpated as a hard ‘knot’ superior to the testicle. Swelling due to a reactive hydrocele may be present, as well as erythema of the scrotal wall. A cremasteric reflex may not be present in patients with torsion [2-4,8,17]. The cremasteric reflex is assessed by gently stroking or pinching the skin of the ipsilateral upper thigh and looking for elevation of the testicle, which is a normal response.
-
- ED evaluation
Testicular torsion can be a clinical diagnosis and typically does not require laboratory or even imaging assessment [4,18]. However, com- plete blood cell count, renal function, electrolytes, and urinalysis may be obtained. The Testicular Workup for Ischemia and Suspected Torsion (TWIST) score can assist in determining the probability of testicular tor- sion and includes nausea/vomiting (1 point), testicular swelling (2 points), hard testis (2 points), absent cremasteric reflex (1 point), and high riding testis (1 point) [19-22]. The first line imaging modality is ul- trasound with Color Doppler assessment of the testicle and spermatic cord up to the internal ring level [23-26]. However, this should not delay Surgical consultation and treatment [2,12,22]. Classically, ultra- sound will demonstrate an enlarged, hyperemic testicle with dimin- ished venous and arterial blood flow compared to the unaffected side (Fig. 2). Doppler evaluation typically reveals decreasED flow velocity and increased Flow resistance in the intratesticular arteries of the torsed testicle [27,28]. Testicular enlargement and hydrocele are often present. A twisted spermatic cord may also be discovered on ultrasound with a spiral pattern known as the whirlpool sign [25].
-
- ED management
Testicular torsion is a surgical emergency. time in the ED is crucial, as patients often present several hours after the initial event, and the salvage rate is most successful within 4-8 h of torsion onset [2,4,12,22,29]. emergent management entails symptomatic manage- ment (e.g., analgesics, antiemetics) and emergent urology consultation for operative management. Surgical evaluation and treatment should not be delayed by further assessment if the diagnosis is strongly suspected [4]. Surgical intervention includes exploration and intraoper- ative detorsion and fixation of the testicles in the operating room [2,4,30]. The specialist will perform a contralateral orchiopexy as well
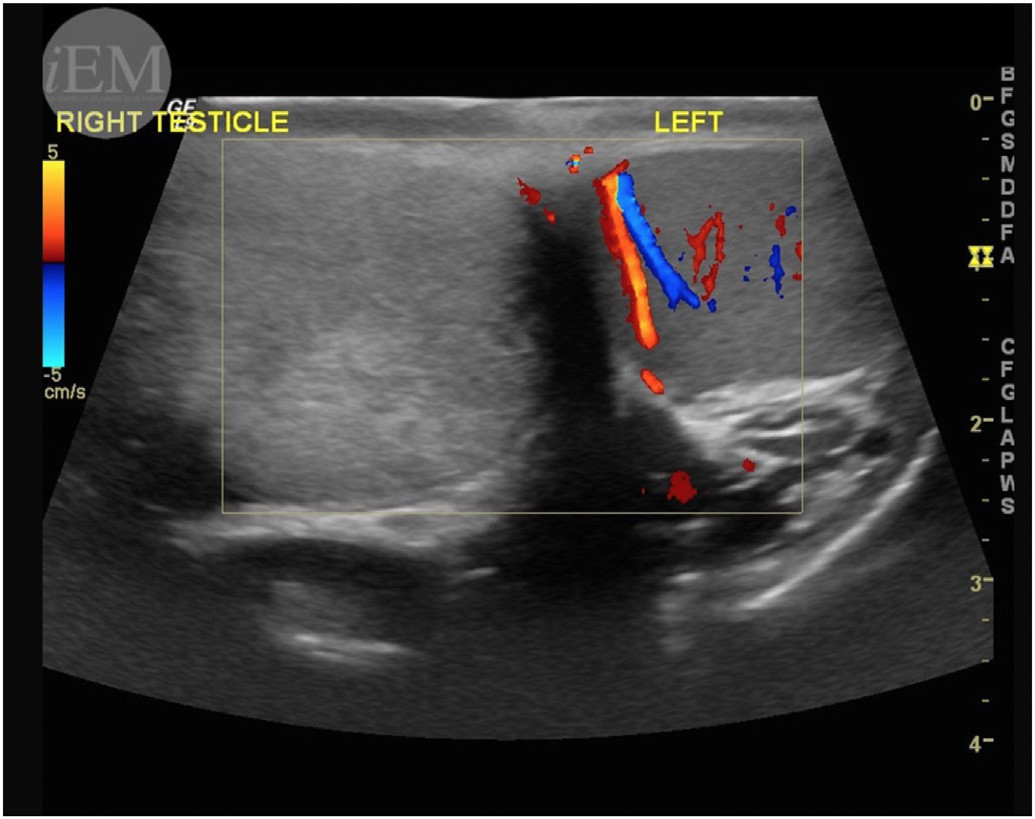
Fig. 2. Ultrasound demonstrating absence of color doppler flow of the right testicle, consis- tent with torsion. Available at https://www.flickr.com/photos/iem-student/43414588252.
history and examination findin”>to prevent future torsion. Prolonged ischemia may result in testicular is- chemia and necrosis, necessitating orchiectomy [2,4,9]. If surgery is not available emergently, manual detorsion is warranted. Testicles classi- cally rotate medially during torsion, and thus detorsion entails rotating the affected testis outward, as if “opening a book” towards the ipsilateral thigh [9,31-33]. Signs of successful detorsion include pain relief, normal anatomic testicle position (i.e., conversion to a longitudinal orientation lower in the scrotum), and normal color Doppler ultrasound [2,4,34].
- Pearls and pitfalls
- What are the high-yield risk factors for testicular torsion?
While all predisposing risk factors for testicular torsion have not been fully elucidated, there are several risk factors that should raise sus- picion for the diagnosis [35]. Anatomic risk factors including the bell- clapper deformity, a defect in which the tunica vaginalis affixes itself to the testicle enabling increased testicular mobility, can predispose to testicular torsion [1,36]. This anatomical defect is bilateral in up to 80% of patients and is assumed to be present contralaterally in all patients with testicular torsion [36,37]. A history of testicular torsion increases the likelihood of torsion in contralateral testicle, and for this reason, sur- gically explored cases of torsion almost always undergo orchiopexy of the contralateral testicle [36,38].
Family history should be considered, as 10% of cases are associated with a positive family history for testicular torsion [1]. Although the pat- tern of inheritance has not been defined [12], obtaining details about the specific age of the torsion event of the affected family member may also be important as there is evidence suggesting “age clustering” within families [39]. Acute trauma has been implicated in 4-10% of cases of tor- sion, and thus clinicians must avoid misdiagnosing Acute scrotal pain as a result of trauma alone [33,39-42].
-
- What history and examination findings are reliable?
There are several history and examination findings that suggest tes- ticular torsion. There is a bimodal age distribution for testicular torsion, and thus age must be a consideration [43]. Peak presentation occurs during the first year of life and 12-18 years of age, though testicular tor- sion can occur at any age [15,43,44].
Pain that is acute in onset is present in 84.3-90% of patients with tes- ticular torsion and is highly associated with the diagnosis [45-48]. This pain is almost exclusively unilateral [48]. Pain <24 h in duration is asso- ciated with an odds ratio (OR) of 6.7 (95% CI 1.54-33.33) [49]. Of note, up to 20% of patients present with no localized testicular pain, but rather abdominal or flank pain alone [8]. History of nausea has positive and negative likelihood ratios of 5 and 0.5, respectively, for diagnosing tor- sion, and thus the absence of nausea should not be used to exclude the diagnosis [22,45,49]. Dysuria and fever may be present but are un- common in patients with testicular torsion (0-12% and 0-20%, respec- tively) [45,46,48].
The most reliable physical examination findings include abnormali- ties to the testicle itself, such as testicular swelling, high riding position, abnormal lie, and firmness [22,46]. A hard testicular mass is associated with testicular torsion (positive likelihood ratio 6.7). However, the pres- ence of a high riding position in isolation is unlikely to be helpful for di-
agnosis (positive likelihood ratio 2.5) [22,49]. Erythema of the scrotal
cannot rely on the presence or absence of a cremasteric reflex when evaluating for testicular torsion. Prehn’s sign (i.e., pain relief with eleva- tion of the testicle) should not alleviate the concern for testicular tor- sion, as one study found that up to 33% of children with surgically confirmed testicular torsion had relief with scrotal elevation [51].
No clinical history or examination factor in isolation can rule out tes- ticular torsion, and all findings should be used in conjunction with screening scores, imaging modalities, and expert consultation to assist with the diagnosis. If the clinician is concerned for testicular torsion based on the history and examination, emergent consultation is recom- mended.
-
- What are mimics of testicular torsion?
There are several disease processes that may cause sudden pain or swelling to the scrotum and thus may mimic testicular torsion (Table 1) [3,52]. History and examination can assist in narrowing the differential diagnosis. Epididymitis, orchitis, and other urinary tract infections can mimic testicular torsion due to pain and are often associ- ated with recent Viral illness and specific tenderness on the epididymis opposed to the testicle itself. sexually transmitted infections are a com- mon cause of epididymitis and testicular discomfort. Of the 2 million sexually transmitted infections diagnosed each year in the U.S., approx- imately half are between the ages 15-24 years, making it a common mimic of testicular torsion in an at-risk age group [53]. History, exami- nation, and urinary studies can help differentiate these diagnoses [54]. Oncologic diagnoses can mimic testicular torsion by causing swelling and mass effect in the scrotum. A diffusely hard testicle can be a sign of testicular or hematologic oncologic disease, such as leukemia or lym- phoma, and may be differentiated from torsion based on laboratory findings, systemic symptoms, and ultrasound [52]. Scrotal swelling caused by idiopathic edema [55], hernia, hydroceles, varicocele, and trauma may also mimic testicular torsion [52]. When evaluating for scrotal swelling caused by idiopathic edema, there is more likely to be edema of the overlying skin leading to loss of scrotal rugation, a feature often absent in swelling secondary to torsion [52,55]. Patients
Table 1
Differential diagnosis of acute testicular pain.
Diagnosis Clinical features
Epididymo-orchitis and infection Tender testicle or epididymis
Recent viral illness Abnormal urinalysis Fever
Hydrocele Transillumination present Positional swelling
Idiopathic scrotal edema No signs of infection
Swelling of overlying scrotal skin
inguinal hernia Fluctuation of swelling with activity and positioning
Oncologic disease abnormal laboratory values, including tumor markers
Diffusely hard testicle (lymphoma and leukemia)
Systemic symptoms
Traumatic pain Ecchymosis and/or visible injury to the scrotum
History and mechanism consistent with trauma
wall may be present but is often absent early in the course of the disease [2,4]. A pathologic (reduced or absent) cremasteric reflex may be asso- ciated with testicular torsion but is not definitive for diagnosis (positive likelihood ratio 2.4) [22,47,49]. The presence of a cremasteric reflex does not rule out torsion, as a pathologic cremasteric reflex is not sensi- tive for the disease, with a wide range of abnormal reflex findings re- ported in confirmed torsion cases (8-50%) [46,50]. To complicate the
Torsion of the appendix testis or appendix epididymis
Torsion of the spermatic cord (testicular torsion)
Blue dot sign
Tenderness over the head of the testis or epididymis
Absent or decreased blood flow on doppler ultrasound
High-riding testicle Acute, unilateral pain Nausea and/or vomiting
Palpable cord abnormality
picture further, there are studies that report the cremasteric reflex is ab- sent in up to 30% of males with normal testicles [8]. Thus, a clinician
Varicocele Dull, aching pain
Fluctuation of pain and swelling
presenting with a hernia will have fluctuation of the swelling and mass with activity and can have an associated groin mass [1]. Hydroceles are typically painless and will transilluminate [56]. Torsion of appendix tes- tis or appendix epididymis, an appendage of normal tissues suspended from the apex of the testis or epididymis, respectively, can be differen- tiated by the blue dot sign (visualization of the inflamed appendage through scrotal skin) and specific tenderness in their anatomical loca- tion on examination [1,57,58]. It is important to note that testicular tor- sion can also cause lower abdominal pain, and Abdominal pathology can also cause testicular pain [59].
When evaluating a patient with testicular pain, emergency clinicians must consider intra-Abdominal emergencies such as appendicitis as well and inquire about other abdominal (i.e., vomiting, diarrhea, disten- sion) and systemic (i.e., fever, chills, rigors) signs and symptoms [60]. Ultimately, testicular torsion may present with a variety of history and examination findings, and there are several mimics. Due to its morbid- ity, testicular torsion must be considered in patients with abdominal or flank pain, nausea, vomiting, and pain in the testicles or scrotum [4,56].
-
- What decision-making rules are available for testicular torsion, and are they reliable?
Several Decision tools are available to assist in the evaluation of tes- ticular torsion. The TWIST score is the most studied clinical decision- making tool, first proposed in 2013 [19] for the evaluation and manage- ment of testicular torsion in children who present with acute testicular pain (Table 2). It has been validated in several independent studies [20,21] and a systematic review in the pediatric population [22].
This scoring system stratifies patients presenting with symptoms concerning for testicular torsion into low, intermediate, and high-risk categories [19]. In the initial development cohort of the TWIST score, the authors reported 100% negative and positive predictive values at the cutoffs of 2 and 5 points, respectively, creating the low and high- risk groups [19]. A score <= 2 points had a negative likelihood ratio of 0, while a score >= 5 had a positive likelihood ratio of infinity [19]. The orig- inal clinical decision rule recommends that patients in the low-risk cat- egory can forgo further ultrasound and specialty consultation, as another diagnosis is more likely. Patients in the intermediate risk cate- gory should undergo ultrasound to evaluate for testicular torsion, and patients in the high-risk category should have emergent specialty con- sultation without delay due to the high likelihood of torsion [19]. Use of the TWIST scoring system could lead to operative management of high-risk torsion patients without ultrasonographic confirmation of the diagnosis, but acceptance of this Management strategy may vary by clinical site and urologist preference.
Subsequent validation studies and systematic reviews of the TWIST score suggest that the initially proposed cutoff values may not be as re- liable as originally discussed [20-22]. In the first validation study recom- mendations for risk stratification cutoffs were suggested as 0 points for the low risk group, 1-5 points for the intermediate risk group, and 6 or greater points for the High risk group [20]. A subsequent validation study published in 2017 found that overall the TWIST score for pediatric patients to have excellent discrimination [21]. In this study, interrater
Table 2 The Testicular Workup for Ischemia and Suspected Torsion (TWIST) scoring and risk strat- ification system [19].
TWIST Score (original Barbosa et al. scoring system)
Testicular swelling (two points) Score 0-2
reliability in calculating the TWIST score had substantial agreement in the components of nausea, scrotal swelling, and high-riding testicle, but less for hard testicle (k = 0.25, 95% CI -0.20 to 0.69) and absent cremasteric reflex (k = 0.52, 95% CI 0.27-0.77) [21]. This 2017 valida- tion study found a likelihood ratio of 0.37 or less with scores <=2, while a score of 7 had a likelihood ratio of infinity for diagnosis [21]. Overall, recalculating the data in studies of the TWIST score suggests a certainty of torsion approaching 100% for patients with a score of 7, although this is limited by only moderate agreement among those applying the TWIST score and additional uncertainty because of the small number of patients in studies with a score of 7 [19-22]. Of note, there was only fair agreement (k = 0.39, 95% CI 0.22-0.46) between clinicians. While clinicians should not use a scoring system in isolation to determine the need for definitive management, patients with an elevated TWIST score should undergo emergent urology specialist evaluation [21].
While testicular torsion is most common in those <18 years [15,43,44], it can occur in adults [61,62]. One study evaluating the TWIST score in adults found high predictive values and advocates its use as a valid decision tool [61,62]. The Boettcher Alert Score (BALS), which has been validated in a two-center study in 2020, has been sug- gested as an easier scoring system to implement as it dichotomizes the likelihood of diagnosis into two categories and has a unified scoring system [45-47].
A 2022 meta-analysis evaluated 5 risk stratification systems and found that Barbosa’s original scoring system was the most reliable over- all [22]. Overall, studies evaluating different scoring systems demon- strate that low-risk groups have a low likelihood of testicular torsion, while high-risk groups have a significant likelihood. However, scoring systems should never be used in isolation, but rather only as a means to supplement clinical assessment and decision making. If the clinician is concerned for testicular torsion based on the history and examination, ultrasound and emergent urology consultation are recommended.
-
- What are the limitations of the evaluation, including ultrasound?
The mainstay of evaluating acute scrotal pain is ultrasound with doppler flow [63]. Ultrasound in adult patients has likelihood ratios as- sociated with a positive and negative test of approximately 26 and 0.1, respectively [23,64]. A systematic review and meta-analysis of ultra- sound in pediatric patients also demonstrated likelihood ratios for a positive and negative test of 33 and 0.02, respectively [64]. It should be noted that patients with a high likelihood of testicular torsion on his- tory and examination or a scoring system should have immediate spe- cialist consultation, as obtaining an ultrasound is associated with diagnostic delay if used inappropriately [14].
Testicular torsion can be classified as complete, partial, or incom- plete. Complete torsion is found when the testis twists 360 degrees or greater [25]. This phenomenon would expect to yield no intratesticular doppler perfusion on ultrasound; however, the flow can be preserved or slightly decreased in patients with complete torsion [25]. Incomplete torsion is when the testicle twists <360 degrees resulting in decreased blood flow to the testis [25]. This can be difficult to diagnose and is heavily dependent on the ultrasonographer, as the symmetry of the testicles and blood flow to each testicle can be subjective [25]. Intermit- tent torsion is defined as sudden onset testicular pain followed by com- plete resolution of pain [25]. Normal testicular flow after a period of decreased or no flow to the testicle can be seen on ultrasound [65,66]. Patients with intermittent torsion are still at risk for developing com- plete torsion. When secondary scrotal inflammation worsens, pain again increases, along with infarction of the testicle [67].
There are several other sonographic signs that can be indicative of
Hard testis (two points)
Absent cremasteric reflex (one point) nausea or vomiting (one point)
High riding testis (one point)
low risk score 3-4
Intermediate risk Score 5-7
High risk
testicular torsion other than the absence of doppler flow. The whirlpool sign of the spermatic cord demonstrates the spermatic cord twisting at the external inguinal ring or within the scrotal sac and is diagnostic of torsion of the spermatic cord and testicle [25]. A mass can form below the point of twisting of the spermatic cord, termed pseudomass. This
pseudomass consists of a congested epididymis, vas deferens, and vas- cular bundle and is often misdiagnosed as epididymitis on ultrasound [65]. Excess and tortuous spermatic cord visualized within the scrotal sac is termed redundant spermatic cord. Redundant spermatic cord can be a sign of an abnormal attachment of the tunica vaginalis. A hor- izontally lying testicle is concerning for abnormal attachment of the tu- nica vaginalis. Globular testicular enlargement from vascular congestion can be concerning for testicular torsion but is often mistaken for orchitis [25]. These ultrasound findings can help diagnose testicular torsion in especially difficult cases when blood flow appears preserved on ultra- sound and the patient appears to be in no pain. However, these ultra- sound findings are often dependent on the ultrasonographer’s skills and experience. A multicenter study reviewed 208 patients with testic- ular torsion proven operatively and found that 24% (50 patients) had normal or increased testicular vascularization on ultrasound [68]. This study found that the radiologist’s training level was the best predictor factor of high-resolution ultrasonography reliability [68].
Intermittent torsion can be challenging to diagnose especially when the patient has no pain. In a retrospective review of intermittent testic- ular torsion, 15 patients were identified accounting for 19 episodes con- cerning for intermittent torsion. All underwent ultrasound to evaluate for testicular torsion [65]. Twelve of the 19 episodes had absent testicu- lar flow on ultrasound followed by normal to increased testicular flow. Five had normal flow, and two had decreased flow. Ten of the 15 pa- tients underwent surgery. Nine were found to have intermittent testic- ular torsion, and one was found to have acute testicular torsion. The patient with acute testicular torsion had documented flow to the af- fected testicular on ultrasound preoperatively. Of the 19 patients with intermittent torsion, 15 had a whirlpool sign or pseudomass on ultra- sound. Two patients had a boggy thickened cord. This study argues that scrotal ultrasound should include careful examination for a whirl- pool sign or pseudomass below the external inguinal ring, especially in patients with Clinical concern for testicular torsion. [65]. This high- lights that normal or increased testicular flow does not rule out acute Surgical pathology, and if there is suspicion for intermittent torsion, con- sultation with the urology specialist is recommended.
Consideration of testicular torsion and early urological consultation is key to ED management. Abrupt onset of scrotal pain, nausea, and vomiting is concerning for testicular torsion. If the clinician is concerned for torsion based on the history and examination, or if a TWIST score of
>6 is present, emergent consultation with possible surgical interven- tion is recommended in the urological literature, rather than waiting for ultrasound evaluation [19,20,22]. Of note, prediction rules are meant to assist in medical decision making, but they are not definitive. Coupled with oftentimes unreliable physical examination findings, cli- nicians should have a low threshold for urology consultation and dopp- ler ultrasound of the scrotum in equivocal cases. Furthermore, if obtained, the ultrasound findings should be considered in combination with the clinical assessment, as normal testicular flow on ultrasound does not definitively exclude testicular torsion [13]. Of note, accelerated torsion Care pathways have demonstrated decreased time from ED eval- uation to surgery and decreased need for orchiectomy [69,70].
Testicular torsion carries a high risk of testicular atrophy and necro- sis if not diagnosed and managed within an appropriate time. Testicular salvage occurs in over 90% of cases if detorsion occurs within 6 h [9,30], and one study demonstrated that for every 10-minute delay in the ED, the likelihood of a nonviable testicle during surgical exploration in- creased by 4.8% [71]. A systematic review evaluating testicular salvage reviewed 30 studies including 2116 patients with testicular torsion. The review found the testicular survival was 97% at 0-6 h, 79% at 7-12 h, 61% at 13-18 h, 43% at 19-24 h, 24% at 25-48 h, and 7% at >48 h [9]. A 7-year retrospective study that reviewed over 2000 cases with
testicular torsion found orchiectomy was performed in up to 32% of tes- ticular cases annually [72].
Immediate urological consultation is the essential component of management [22]. If immediate urological consultation is not available, the clinician should attempt manual detorsion [9,31-33]. This entails ro- tating the abnormal testicle medially to laterally, a maneuver termed “opening the book”, with the goal to restore perfusion and improve pa- tient’s pain [13]. The average degree of testicular torsion is cited at 720 degrees but can vary between 180 and 1080 degrees [33]. The range of manual detorsion should be based on pain relief and return of flow as seen on ultrasound [33,34]. If the patient has no relief of pain or sudden increase in pain, the affected testicle should then be rotated in a lateral to medial manner, as up to one third of patients will experience torsion in a medial to lateral manner [33]. Despite this bedside procedure, any patient with concern for testicular torsion warrants emergent urological evaluation, even if symptoms are relieved. One group of authors argue that any pediatric patient presenting with testicular pain warrants sur- gical exploration to ensure no testicular torsion [73], although this is not standard of care in society guidelines [74]. A study at a tertiary surgical center retrospectively reviewed 121 pediatric patients under the age of 15 years old who presented with acute scrotal pathology, excluding pa- tients with inguinal hernias, hydroceles, and neonatal extravaginal tor- sion [73]. Of the 121 patients with acute scrotal pathology, 113 underwent Exploratory surgery. Thirty-one of these patients (27%) were found to have testicular torsion, 64 (57%) had a torsed appendage testis, 12 (11%) had epididymitis, 1 (1%) had fat necrosis, and 5 (4%) had no abnormality noted. Eight patients required orchiectomy. Of these eight patients, two patients with testicular torsion had no pain but a tender testicle, and one had a normal scrotal ultrasound examination. Three of the eight patients had a normal cremasteric reflex. A true pos- itive ultrasound finding of testicular torsion was only found in four of the patients with testicular torsion. This study demonstrates testicular torsion is a difficult diagnosis with unreliable physical examination and ultrasound findings and argues that surgical exploration is manda- tory for any patient if there is concern for testicular torsion [73].
Testicular torsion is painful and uncomfortable, and analgesia, in- cluding parenteral opioids, should be administered in the ED, along with antiemetics if the patient is nauseous or vomiting [13].
Of note, if a patient is deemed appropriate for discharge after ED as- sessment and symptomatic management, strict return precautions should be discussed with the patient, in particular if pain were to recur. short-term follow-up for repeat evaluation or a return timeline is also recommended.
-
- What medicolegal considerations are associated with testicular torsion?
Testicular torsion is the third most common cause of medical mal- practice suits in males aged 12-17 with an average settlement of
$60,000 [8,67]. Atypical presentation and false negative ultrasounds contribute to delayed and missed diagnosis [8]. In one case, a 16-year- old presented to the ED with Right lower quadrant pain, nausea, and vomiting. Concerned for appendicitis, the emergency clinician per- formed laboratory testing, ultrasound of the abdomen, and computed tomography of the abdomen and pelvis (CTAP), which were all reassuring. A general surgeon was consulted for bedside evaluation and deemed appendicitis less likely to be the diagnosis, and the patient was ultimately discharged home. The patient returned to the ED the next day with right testicular pain and was found to have testicular tor- sion. The patient was taken to the OR and underwent a right orchiec- tomy. A lawsuit was filed against the initial emergency clinician for failure to perform a testicular examination and consider testicular tor- sion during the patient’s initial visit. The plaintiff argued isolated ab- dominal pain is often a common presenting symptom of testicular torsion. The case was settled for $300,000 [67]. In a review of 53 testic- ular torsion malpractice cases, 31% of patients presented with
abdominal pain only [75]. Emergency clinicians should continue to con- sider testicular torsion in atypical presentations, routinely document a scrotal examination in younger males who present with abdominal pain, and have a low threshold for Ultrasound imaging and prompt urol- ogy consultation [67].
A similar outcome occurred in the medical litigation case Graham v. Noreldin in which a 14-year-old male presented to the ED with abdom- inal pain [67]. Laboratory testing was reassuring, but a CTAP demon- strated findings suggestive of appendicitis. The emergency clinician obtained a surgical consultation who determined appendicitis was un- likely. An ultrasound of the scrotum was then obtained, which was interpreted as epididymitis. The patient was discharged with antibi- otics. Three days later, the patient presented to a different ED with tes- ticular pain. The patient was diagnosed with testicular torsion and underwent orchiectomy. A review of the initial ultrasound revealed de- creased testicular flow. A case was filed against the initial emergency clinician, not the radiologist. The jury awarded the patient $500,000, as the emergency clinician can make a clinical correlation with the ul- trasound interpretation that a radiologist cannot [67]. This highlights that the emergency clinician should clinically correlate ultrasound find- ings with the history and physical examination.
-
- What lessons learned do testicular torsion and Ovarian torsion have in common?
Testicular torsion and ovarian torsion are challenging diagnoses given unreliable physical examination findings, intermittent torsion pathophysiology, and limitations of ultrasound findings [76]. Similar to intermittent ovarian torsion, intermittent testicular torsion can be misdiagnosed or have a delayed diagnosis with a false negative ultra- sound and reassuring examination when the patient is not experiencing torsion or symptoms at the time of the ED evaluation [76]. Similar to ovarian torsion, specific age ranges are more likely to suffer from the condition, and in both ovarian torsion and testicular torsion, those with anatomical variations such as an adnexal mass and the bell clapper deformity, respectively, are more likely to develop torsion [36,76]. The presentations of testicular and ovarian torsion can mimic a broad differ- ential of pathology which can easily persuade a clinician to pursue an in- fectious process or intra-abdominal source [77]. The diagnosis often depends on the clinician’s gestalt and decision to obtain surgical consul- tation [76,77]. Both testicular and ovarian torsion diagnoses are time sensitive and warrant early surgical consultation [76,77], and both are a source of medical litigation given the high rate of complications with delayed or missed diagnoses [77]. Unlike ovarian torsion, scoring sys- tems such as the TWIST score can help provide a framework for the
Testicular torsion pearls.
- The peak age of testicular torsion is 12-18 years of age, but all ages may be affected.
- Trauma is associated with 4-10% of testicular torsion cases.
- No finding on history or examination may exclude testicular torsion. A normal cremasteric reflex does not reliably exclude testicular torsion.
- Patients, especially adolescents, presenting with lower abdominal pain or nausea and vomiting should undergo a testicular examination to rule out testicular pathology.
- The TWIST score has been validated and can help guide clinical decision mak- ing in patients presenting with acute testicular pain.
- Doppler ultrasound can aid in diagnosis and is sensitive and specific. However, it can be falsely negative. Thus, clinical judgment should supersede a negative ultrasound finding.
- Testicular torsion is a time-sensitive diagnosis, and patients presenting with acute testicular pain require an expedited evaluation and early consultation with the urology specialist if there is concern or confirmed testicular torsion.
- Testicular torsion related issues are a common cause of Medical malpractice
suits, and clinicians should prudently evaluate and document on all patients who present with lower abdominal or testicular pain their concerns and give strict return precautions if discharging the patient.
evaluation of testicular torsion [22], but if the emergency clinician is highly suspicious of either condition based on the history and examination, emergent consultation with the surgical specialist is recommended.
Table 3 lists pearls and pitfalls in the evaluation and management of testicular torsion.
- Conclusions
Testicular torsion occurs with complete or partial rotation of the tes- ticle leading to obstruction of vascular flow which can result in testicu- lar demise if not emergently corrected. Risk factors for the disease include anatomic deformities such as the bell clapper deformity. Neo- nates and children aged 12-18 are the most common patients affected, although 14% of all testicular torsion cases are in adults. Acute, unilateral testicular pain is the most common symptom, and testicular torsion is often associated with nausea and vomiting. Relying on the presence or absence of the cremasteric reflex is not a reliable method for ruling in or out testicular torsion. The TWIST scoring system can be used to help guide clinical management. Doppler ultrasound is both sensitive and specific for the diagnosis of torsion and can aid in diagnosis, but it may be falsely negative. Thus, clinical judgment is necessary. If the his- tory and examination are concerning for torsion, emergent surgical con- sultation is necessary without delay, as the diagnosis is time sensitive. Treatment includes urology consultation for evaluation and detorsion of the testicle, along with symptom control in the ED.
CRediT authorship contribution statement
Aaron Lacy: Writing – review & editing, Writing – original draft, Vi- sualization, Validation, Conceptualization. Amanda Smith: Writing – review & editing, Writing – original draft, Visualization, Validation. Alex Koyfman: Writing – review & editing, Visualization, Validation, Supervision, Conceptualization. Brit Long: Writing – review & editing, Writing – original draft, Validation, Supervision, Conceptualization.
Declaration of Competing Interest
None.
Acknowledgements
AL, AS, BL, and AK conceived the idea for this manuscript and con- tributed substantially to the writing and editing of the review. This man- uscript did not utilize any grants, and it has not been presented in abstract form. This clinical review has not been published, it is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, includ- ing electronically without the written consent of the copyright-holder. This review does not reflect the views or opinions of the U.S. govern- ment, Department of Defense, U.S. Army, U.S. Air Force, or SAUSHEC EM Residency Program.
References
- Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and manage- ment. Am Fam Phys. 2013;88(12):835-40.
- Laher A, Ragavan S, Mehta P, Adam A. Testicular torsion in the emergency room: a review of detection and management strategies. Open Access Emerg Med. 2020; 12:237-46.
- Ta A, D’Arcy F, Hoag N, D’Arcy J, Lawrentschuk N. Testicular torsion and the acute scrotum: current emergency management. Eur J of Emerg Med. 2016;23(3):160-5.
- Rosenberg H, Long B, Keays M. Just the facts: assessment and management of testic- ular torsion in the emergency department. CJEM. 2021;23(6):740-3.
- Korkes F, Cabral P, Moro Alves C, Savioli M, Pompeo A. Testicular torsion and Weather conditions: analysis of 21,289 cases in Brazil. Int Braz J Urol. 2012;38(2): 222-8.
- Fujita N, Tambo M, Okegawa T, et al. Distinguishing testicular torsion from torsion of the appendix testis by clinical features and signs in patients with acute scrotum. Res Rep Urol. 2017;9:169-74.
- Stephenson GS, Langdorf MI. Testicular torsion appearance and diagnosis on com- puted tomography of the abdomen and pelvis: case report. Clin Pract Cases Emerg Med. 2022;6(2):117-20.
- Mellick L. Torsion of the testicle: it is time to stop tossing the dice. Pediatr Emerg Care. 2012;28(1):80-6.
- Mellick LB, Sinex JE, Gibson RW, Mears K. A systematic review of testicle survival time after a torsion event. Pediatr Emerg Care. 2019;35(12):821-5.
- Bowlin PR, Gatti JM, Murphy JP. Pediatric testicular torsion. Surg Clin North Am. 2017;97(1):161-72.
- Nassiri N, Zhu T, Asanad K, Vasquez E. Testicular torsion from Bell-clapper deformity.
- Osumah TS, Jimbo M, Granberg CF, Gargollo PC. Frontiers in pediatric testicular tor- sion: an integrated review of prevailing trends and management outcomes. J Pediatr Urol. 2018;14(5):394-401.
- Schick Michael, Sternard Britni. Testicular torsion. StatPearls [Internet]. 2022..
- Chan EP, Wang PZT, Myslik F, Chen H, Dave S. Identifying systems delays in assess- ment, diagnosis, and operative management for testicular torsion in a single-payer health-care system. J Pediatr Uro. 2019;15(3):251.e1-7.
- Zhao L, Lautz T, Meeks J, Maizels M. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward im- proving the quality of care. J Urol. 2011;186(5):2009-13.
- Cummings JM, Boullier JA, Sekhon D, Bose K. Adult testicular torsion. J Urol. 2002; 167(5):2109-10.
- Schmitz D, Safranek S. Clinical inquires. How useful is a physical exam in diagnosing testicular torsion? J Fam Prac. 2009;58(8):433-4.
- Aihole JS. Testicular torsion; clinical diagnosis or imaging diagnosis? Radiol Case Rep. 2022;17(8):2665-7.
- Barbosa J, Tiseo B, Barayan G, et al. Development and initial validation of a scoring system to diagnose testicular torsion in children. J Urol. 2013.;189(5) (1859-1854).
- Sheth K, Keays M, Grimsby G, et al. Diagnosing testicular torsion before urological consultation and imaging: validation of the TWIST score. J Urol. 2016;195(6): 187-1876.
- Frohlich L, Paydar-Darian N, Cilento Jr B, Lee L. Prospective validation of clinical score for males presenting with an acute scrotum. Acad Emerg Med. 2017;24(12): 1474-82.
- Qin K, Qu L. Diagnosing with a TWIST: systemic review and meta-analysis of a tes- ticular torsion risk score. J Urol. 2022;208(1):62-70.
- Ota K, Fukui K, Oba K, et al. The role of ultrasound imaging in adult patients with tes- ticular torsion: a systematic review and meta-analysis. J Med Ultrason (2001). 2019; 46(3):325-34.
- Vijayaraghavan SB. Sonographic differential diagnosis of acute scrotum: real-time whirlpool sign, a key sign of torsion. J Ultrasound Med. 2006;25(5):563-74.
- Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018;48(5):735-44.
- Pepe P, Panella P, Pennisi M, Aragona F. Does color Doppler sonography improve the clinical assessment of patients with acute scrotum? Eur J Radiol. 2006;60(1):120-4.
- Prando D. Torsion of the spermatic cord: the main gray-scale and doppler sono- graphic signs. Abdom Imaging. 2009. [Sep-Oct. 34 (5):648-61].
- Expert Panel on Urological Imaging, Wang CL, Aryal B, Oto A, Allen BC, Akin O, et al. ACR appropriateness criteria(R) acute onset of scrotal pain-without trauma, without antecedent mass. J Am Coll Radiol. 2019;16(5S):S38-43.
- Zvizdic Z, Aganovic A, Milisic E, et al. Duration of symptoms is the only predictor of testicular salvage following testicular torsion in children: a case-controlled study. Am J Emerg Med. 2021;41:197-200.
- Pogorelic Z, Mustapic K, Jukic M, et al. Management of acute scrotum in children: a 25-year single center experience on 558 pediatric patients. Can J Urol. 2016;23(6): 8594-601.
- Friedman A, Palmer L, Maizels M, Bittman M, Avarello J. Pediatric acute scrotal pain: a guide to patient assessment and triage. J Pediatr Urol. 2016;12(2):72-5.
- Fantasia J, Aidlen J, Lathrop W, Ellsworth P. Undescended testes: a clinical and surgi- cal review. Urol Nurs. 2015;35(3):117-26.
- Sessions AE, Rabinowiz R, Hulburt WC, Goldstein MM, Mevorach RA. Testicular tor- sion: direction, degree, duration and disinformation. J Urol. 2003;169(2):663-5.
- Vasconcelos-Castro S, Flor-de-Lima B, Campos J, Soares-Oliveira M. Manual detorsion in testicular torsion: 5 years of experience at a single center. J Pediatr Surg. 2020;55(12):2728-31.
- Tabakin A, Farber N, Barone J. Testicular torsion in brothers. Can J Urol. 2020;27(1): 10135-7.
- Favorito LA, Cavalcante AG, Costa WS. Anatomic aspects of epididymis and tunica vaginalis in patients with testicular torsion. Int Braz J Urol. 2004;30:420-4.
- Mansbach JM, Forbes P, Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159(12):1167-71.
- Bolin C, Driver CP, Youngson GG. Operative management of testicular torsion: cur- rent practice within the UK and Ireland. J Pediatr Urol. 2006;2(3):190-3.
- Shteynshlyuger A, Yu J. Familial testicular torsion: a meta analysis suggests inheri- tance. J Pediatr Urol. 2013;9(5):683-90.
- Zhong H, Bi Y. Pediatric trauma-induced testicular torsion: a surgical emergency. Urol Int. 2021;105(3-4):221-4.
- Seng YJ, Moissinac K. Trauma induced testicular torsion: a reminder for the unwary. J Accid Emerg Med. 2000;17(5):381-92.
- Waldert M, Latte T, Schmidbauer J, et al. Color doppler sonography reliably identifies testicular torsion in boys. Urol. 2010;75(5):1170-4.
- Shunmugam M, Goldman RD. Testicular torsion in children. Can Fam Physician. 2021;67(9):669-71.
- Lee SM, Huh JS, Baek M, et al. A nationwide Epidemiological study of testicular tor- sion in Korea. J Korean Med Sci. 2014;29(12):1684-7.
- Klinke M, Elrod J, Stiel C, et al. The BAL-score almost perfectly predicts testicular tor- sion in children: a two-center cohort study. Front Pediatr. 2020;7(8):601892.
- Boettcher M, Bergholz R, Kerbs TF, Wenke K, Aaronson DC. Clinical predictors of tes- ticular torsion in children. Urol. 2012;79:670-4.
- Boettcher M, Krebs T, Bergholz R, et al. Clinical and sonographic features predict tes- ticular torsion in children: a prospective study. BJU Int. 2013;112(8):1201-6.
- Sazgar M, Montazer S, Hosseininejad S, et al. Clinical predictors of testicular torsion in patients with acute scrotum; a cross-sectional study. Arch Acad Emerg Med. 2022; 10(1):e9.
- Beni-Israel T, Goldman M, Chaim SB, Kozer E. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Medicine. 2010;28(7):786-9.
- Karmazyn B, Steinbert R, Kornreich L, et al. Clinical and Sonographic criteria of acute scrotum in children: a retrospective study of 172 boys. Pediatr Radiol. 2005;35(3): 302-10.
- Roth B, Giannakis I, Ricklin M, Thalmann G, Exadaktylos A. An accurate diagnostic pathway helps to correctly distinguish between the possible causes of acute scro- tum. Oman Med J. 2018;33(1):55-60.
- Gatti J, Murphy J. Current management of the acute scrotum. Semin Pediatr Surg. 2007;16:58-63.
- Smith L, Angarone M. Sexually transmitted infections. Urol Clin N Am. 2015;42(4): 507-18.
- Trojan T, Lishnak T, Heiman D. Epididymitis and orchitis: an overview. Am Fam Phy-
- Santi M, Lava SAG, Simonetti GD, Bianchetti MG, Milani GP. Acute idiopathic scrotal edema: systematic literature review. Eur J Pediatr Surg. 2018;28(3):222-6.
- Keays M, Rosenberg H. Testicular torsion. CMAJ. 2019;191(28):E792.
- Mushtaq I, Fung M, Glasson MJ. Retrospective review of paediatric patients with acute scrotum. ANZ J Surg. 2003;73(1-2):55-8.
- Lev M, Ramon J, Mor y, Jacobson JM, Soudack M.. sonographic appearances of torsion of the appendix testis and appendix epididymis in children. J Clin Ultrasound. 2015; 43(8):485-9.
- Vasconcelos-Castro S, Soares-Oliveira M. Abdominal pain in teenagers: beware of testicular torsion. J Pediatr Surg. 2020;55(9):1933-5.
- Sieger N, Quilio F, Stolzenburg J. What is beyond testicular torsion and epididymitis? Rare differential diagnosis of acute scrotal pain in adults: a systematic review. Ann Med Surg (Lond). 2020;29(55):265-74.
- Greear G, Romano M, Katz M, Munarriz R, Rague J. Testicular torsion: epidemiolog- ical risk factors for orchiectomy in pediatric and adult patients. Int J Impot Res. 2021; 33(2):184-90.
- Barbosa J, de Freitas P, Carvalho S, et al. Validation of the TWIST score for testicular torsion in adults. Int Urol Nephrol. 2021;53(1):7-11.
- Bourke MM, Silverberg J. Acute Scrotal Emergencies. Emerg Med Clin North Am. 2019;37(4):593-610.
- Mori T, Ihara T, Nomura O. Diagnostic accuracy of point-of-care ultrasound for pae- diatric testicular torsion: a systematic review and meta-analysis. Emerg Med J. 2022. [emermed-2021-212281].
- Munden M, Williams L, Zhang W, et al. Intermittent testicular torsion in the pediatric patient: sonographic indicators of a difficult diagnosis. Am J Roentgenol. 2013;201 (4):912-8.
- Mellick LB, Sinex J. Testicular torsion pain honeymoons. Pediatr Emerg Care. 2019;35 (12):e241-4.
- Bass JB, Couperus KS, Pfaff JL, Moore GP. A pair of testicular torsion medicolegal cases with caveats: the Ball’s in your court. Clin Pract Cases Emerg Med. 2018;2(4):283-5.
- Kalfa N, Veyrac C, Lopez M, et al. Multicenter assessment of ultrasound of the sper- matic cord in children with acute scrotum. J Urol. 2007;177(1):297-301.
- Zee RS, Bayne CE, Gomella PT, et al. Implementation of the accelerated care of tor- sion pathway: a quality improvement initiative for testicular torsion. J Pediatr Urol. 2019;15(5):473-9.
- Romao RLP, Anderson KH, MacLellan D, Anderson P. Point-of-care influences orchi- ectomy rates in pediatric patients with testicular torsion. J Pediatr Urol. 2019.;15(4) (367.e1-367.e7).
- Gold DD, Lorber A, Levine H, et al. Door to detorsion time determines testicular sur- vival. Urology. 2019;133:211-5.
- Cost NG, Bush NC, Barber TD, Huang R, Baker LA. Pediatric testicular torsion: demo- graphics of national orchiopexy versus orchiectomy rates. J Urol. 2011;185:2459-63.
- Murphy FL, Fletcher L, Pease P. Early scrotal exploration in all cases is the investiga- tion and intervention of choice in the acute paediatric scrotum. Pediatr Surg Int. 2006;22(5):413-6.
- Thakkar HS, Yardley I, Kufeji D. Management of paediatric testicular torsion – are we adhering to royal college of surgeons (RCS) recommendations. Ann R Coll Surg Engl. 2018;100(5):397-400.
- Gaither TW, Copp HL. State appellant cases for testicular torsion: case review from 1985 to 2015. J Pediatr Urol. 2016;12(5):291.e1-5.
- Bridwell RE, Koyfman A, Long B. High risk and low prevalence diseases: ovarian tor- sion. Am J Emerg Med. 2022;56:145-50.
- Robertson JJ, Long B, Koyfman A. Myths in the evaluation and management of ovar- ian torsion. J Emerg Med. 2017;52(4):449-56.
