Initial evaluation and management of wide-complex tachycardia: A simplified and practical approach
a b s t r a c t
The evaluation and treatment of wide QRS-complex tachycardia remains a challenge, and mismanagement is quite common. Diagnostic aids such as wide-complex tachycardia algorithms perform poorly in the real-life set- ting. The purpose of this review is to offer a simple clinical-electrocardiographic approach for the initial evalua- tion and management of the adult patient with stable wide-complex tachycardia that does not require recollection of complex guidelines or algorithms.
(C) 2019
Is the tachycardia regular or irregular?
Sustained wide-complex tachycardia (WCT), that is, WCT recorded in a 12-lead electrocardiogram , is a common presentation in the emergency department and in other acute-care settings. The differ- ential diagnosis includes Ventricular tachycardia and supraventric- ular tachycardia (SVT), including atrial fibrillation, with Aberrant intraventricular conduction. Aberrant conduction of SVT comprises Right bundle branch block (RBBB), Left bundle branch block , non- specific intraventricular conduction block and ventricular preexcitation as seen in the Wolff-Parkinson-White (WPW) syndrome [1,2]. Under specific clinical circumstances, metabolic abnormalities such as Severe hyperkalemia or sodium-channel blocker toxicity may also manifest as WCT in the ECG [3]. As the treatment of the listed conditions is vastly different, reaching a quick and accurate diagnosis is paramount. Several studies have shown that diagnostic aids such as WCT algorithms per- form poorly at the bedside with resultant misdiagnosis, mismanage- ment and potential harm to the patient [1,4,5]. The purpose of this review is to provide the clinician with a simple, clinically-oriented method that does not require sophisticated knowledge of the ECG or recollection of complex guidelines and algorithms. Fig. 1 summarizes our approach to the diagnosis and management of the adult emergency department patient with stable WCT.
* Corresponding author at: Department of Internal Medicine, Carolinas Medical Center,
P.O. Box 32861, Charlotte, NC 28232, United States.
E-mail address: [email protected] (L. Littmann).
This should be a relatively easy distinction which only requires a brief review of the ECG. Even irregular tachycardias have regular por- tions but if there are any obvious irregular segments, the WCT should be considered to be irregular. It is important to understand that the faster the heart rate, the less irregularity one can expect. In less than ob- vious cases, the use of a caliper is encouraged for the assessment of reg- ularity vs. irregularity.
Regular wide-complex tachycardia
Clinical likelihoods
Although estimations vary regarding the percentage of patients with regular WCT having SVT or VT, it is generally believed that approxi- mately 80% of all regular WCTs are VT [2,6-12]. Most studies that established this high likelihood of VT, however, were done at cardiology referral centers. Unfortunately, there are no prospective studies on WCT cases in the emergency department setting where the percentage of pa- tients with VT is probably lower. Nevertheless, most experts believe that in patients with structural heart disease, a history of myocardial infarc- tion, angina or systolic heart failure, the majority of WCT cases are VT (Fig. 1) [1,2,6-12]. It is important to recognize that WCT algorithms are too complex to be easily recalled by the acute care provider [13- 15]. In addition, their accuracy in the real-life setting ranges from 60 to 75% [7,16-19]. The use of WCT algorithms, therefore, is less useful than establishing the clinical likelihood. Adult advanced cardiac life
https://doi.org/10.1016/j.ajem.2019.04.027
0735-6757/(C) 2019
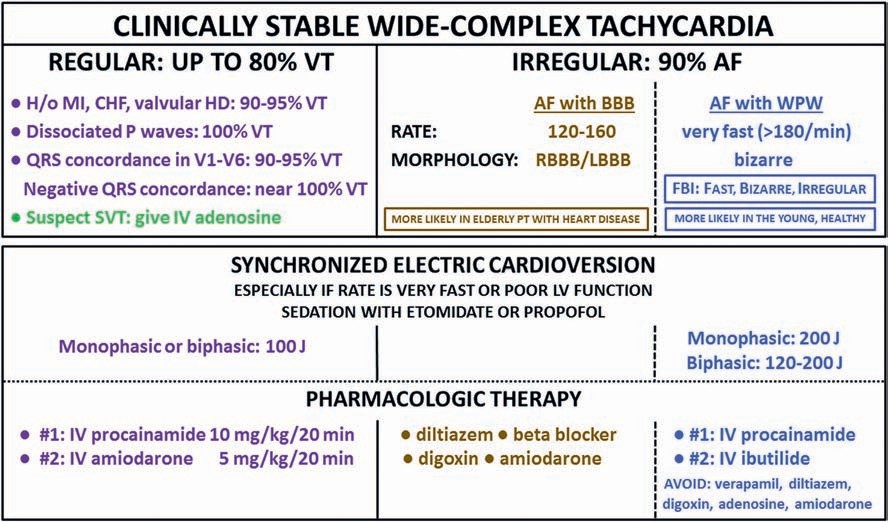
Fig. 1. Combined clinical and electrocardiographic approach to the initial evaluation and management of the adult patient with clinically stable wide-complex tachycardia (WCT). Abbreviations: AF = atrial fibrillation; BBB = bundle branch block; CHF = chronic heart failure; HD = heart disease; IV = intravenous; LBBB = left bundle branch block; MI = myocardial infarction; PO = oral route; PT = patient; RBBB = right bundle branch block; SVT = supraventricular tachycardia; VT = ventricular tachycardia; WPW = Wolff- Parkinson-White syndrome.
support (ACLS) guidelines, appropriately, do not recommend the use of WCT algorithms [20].
Electrocardiographic diagnosis
Based on the listed clinical likelihoods, the default diagnosis of WCT should be “probable VT until proven otherwise [1,9].” Simple ECG obser- vations can further increase the probability of VT (Fig. 1). If an
inconsistent P-QRS relationship is present such as in atrioventricular (AV) dissociation, the WCT is almost certainly VT [1,9,10,21]. In our ex- perience, approximately half of the cases of VT demonstrate visible AV dissociation. It is always useful to spend one or two minutes with the help of a caliper to find sharp “notches” indicative of P waves in one of the rhythm strips as proof of an inconsistent P-QRS relationship (Figs. 2-4). If AV dissociation cannot be ascertained, a simple QRS morpholog- ical sign will still make the diagnosis of VT very likely: the presence of
Fig. 2. ECG recorded from a 62-year-old woman with dilated cardiomyopathy who presented with a 2-day history of heart failure exacerbation. By numerous consecutive providers, the ECG was read as sinus tachycardia with bifascicular block. Red arrows indicate what were believed to be sinus P waves. This case highlights several clinical and ECG traps including diagnostic anchoring, the “P-wave trap” and the “QRS morphology trap” (see text). It was ignored that in a patient with heart failure, WCT almost always represents ventricular tachycardia (VT). In an enlarged lead V1 dissociated P waves are clearly visible (blue arrows) firmly establishing the diagnosis of VT. QRS concordance is also present.
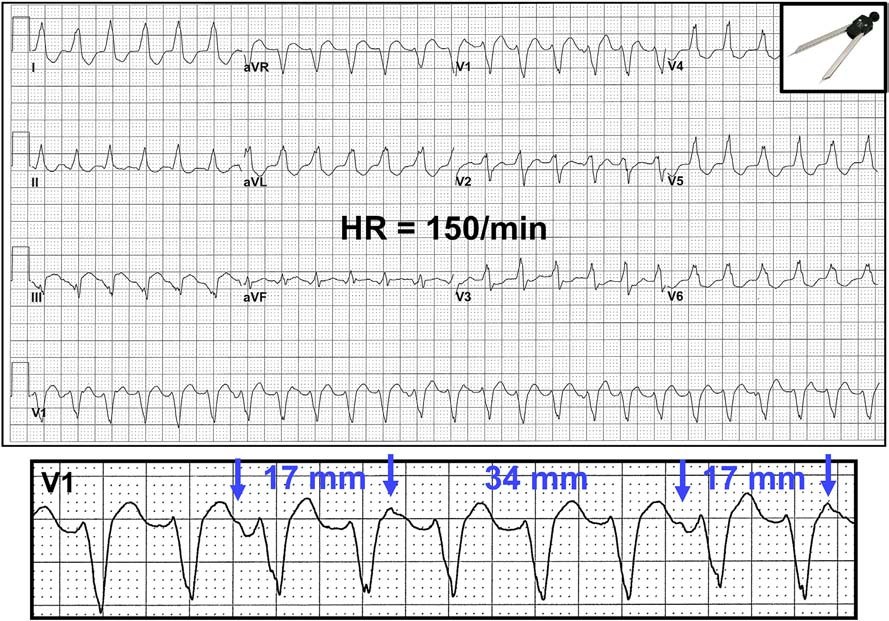
Fig. 3. ECG recorded from a 74-year-old man with remote history of inferior MI who presented with a 4-day history of palpitation and mild shortness of breath. In the emergency department, he was tachycardic but in no distress. By numerous consecutive providers, the ECG was read as tachycardia with left bundle branch block (diagnostic anchoring and the “QRS morphology trap”- see text). In a patient with history of MI, however, 90-95% of WCTs is VT. In the enlarged lead V1 on the bottom dissociated P waves are clearly visible (arrows) firmly establishing the diagnosis of VT.
QRS concordance in the chest leads (i.e., in all six chest leads the QRS complexes go in the same direction, either up or down) (Fig. 2). A neg- ative QRS concordance almost always signifies VT (Fig. 1) [1,10,21,22]. During WCT, one can occasionally detect the presence of QRS com- plexes that are narrower and have a more normal morphology than that of the wide-QRS beats. These are fusion beats. Fusion beats denote ventricular activation from two separate sites. In regular WCT, fusion beats are essentially diagnostic of VT as they reflect simultaneous
ventricular activation from a ventricular site (the VT) and from con- ducted atrial impulses (Fig. 4) [23].
Clinical and ECG traps to avoid
A common clinical trap that frequently results in misdiagnosis is au- tomatically adopting a previous clinician’s false diagnosis (cognitive
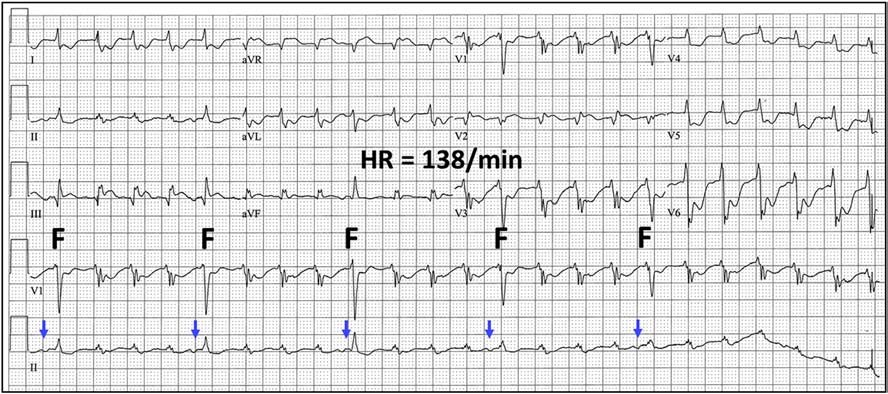
Fig. 4. ECG recorded from a 57-year-old woman with end-stage liver disease and upper GI bleed. Because of suspected supraventricular tachycardia, IV adenosine was administered three times, with no success. The tachycardia finally converted with Electric shock. Note the presence of fusion complexes (F) whose morphology is more normal than that of the other beats. Each fusion complex is preceded by a P wave (blue arrows); this finding also established A-V dissociation and confirmed the diagnosis of VT.
transfer or anchoring) (Figs. 2 and 3). When dealing with WCT, each provider should independently assess the clinical and ECG likelihoods of SVT and VT. The second clinical trap is stating that “the patient is too well for the tachycardia to be VT” (Fig. 3). Patients with VT can be clinically stable on presentation; instability is frequently the result of a missed diagnosis and inappropriate treatment [1,4,5,9,10]. One of the ECG traps to avoid is the “P-wave trap,” focusing too much on a possible 1:1 P-QRS relationship (Fig. 2). First, true 1:1 P-QRS relationship can be due to the occasional patient with VT who has 1:1 retrograde conduc- tion. Second, one can never be sure that what appear to be P waves is not part of the ST-T segments (Fig. 2). The second ECG trap is the “QRS morphology trap” when the first responder prematurely focuses on the QRS morphology during WCT (Figs. 2 and 3). As we have seen, the clinical scenario and the finding of AV dissociation should supersede the finding of a resemblance of the QRS complexes to bundle branch blocks or bifascicular blocks. The combination of a younger, healthier patient whose ECG suggests a 1:1 P-QRS relationship and typical bundle branch block morphology does increase the likelihood of SVT, but one still cannot be certain.
Therapy
If SVT is suspected, as in the scenario discussed above, conversion with intravenous (IV) adenosine strongly supports that assessment (Fig. 1) [24]. If rapid IV push of an appropriate dose of adenosine does not terminate the WCT, it should be considered to be probable VT (Fig. 4) [25]. In questionable cases the use of IV adenosine can be very help- ful: if the cause of WCT is uncertain, it can help define the correct diag- nosis, and if the diagnosis turns out to be SVT, then adenosine is actually the most appropriate treatment of choice. It should be noted that a small percentage of VTs can also be converted with adenosine, so while this medication can be useful diagnostically, a successful application of adenosine does not completely exclude VT [26]. From the perspective of the acute care provider, however, the most important fact is that the tachycardia terminated. Moreover, the use of IV adenosine in WCT has been shown to be safe, regardless of SVT or VT [26].
In WCT that is presumed to be VT (and this is the vast majority of cases), patients who appear to be unstable should undergo direct cur- rent electric cardioversion. Electric cardioversion is also a reasonable first line treatment for stable patients with WCT, especially when the heart rate is very fast or when Bedside echocardiography identifies poor left ventricular systolic function (Fig. 1). As we will see, pharmaco- logic cardioversion takes time, whereas electric cardioversion can be ap- plied almost immediately. Also, the success rate of electrical cardioversion for stable VT is approximately 95%, much higher than the success rate of pharmacological cardioversion [27]. For sedation, etomidate or propofol are the preferred agents (Fig. 1) [28]. The recom- mended energy for cardioversion in regular WCT is 100 joules, regard- less of monophasic or biphasic shock (Fig. 1) [20].
In clinically stable patents with WCT, ACLS allows one attempt at pharmacologic cardioversion. Outside of the acute myocardial infarction setting, lidocaine is one of the least effective agents for conversion of VT. In contrast to widespread beliefs, IV procainamide is both more effective and is safer than IV amiodarone for the acute conversion of VT (Fig. 1) [25,29]. In a recent double-blind randomized trial, IV procainamide at a dose of 10 mg/kg given over 20 min (a dose that is lower than typically used in the United States) converted approximately two thirds of WCTs, whereas IV amiodarone administered as 5 mg/kg over 20 min (a dose higher than typically used in the United States) only converted one third of the tachycardias [25]. Major cardiovascular side effects were much less common with procainamide than with amiodarone [25]. Of note, IV procainamide is the only agent that carries a class IIA indication for the Pharmacologic conversion of VT. As such, in the ACLS guidelines IV procainamide is listed ahead of IV amiodarone [20]. On the other hand, IV amiodarone is the most effective agent in preventing recur- rences of VT, and therefore, its use in repetitive VT is appropriate [20].
Frequently, IV procainamide is used for the termination of VT, followed by IV amiodarone for the prevention of recurrence. The safety of admin- istering procainamide and amiodarone in sequence, however, has not been clearly established.
Irregular wide-complex tachycardia
Clinical-electrocardiographic diagnosis
In contrast to regular WCTs, sustained irregular WCT is almost never VT (Fig. 1). Here, the default diagnosis should be Atrial fibrillation with bundle branch block, nonspecific intraventricular conduction block or ventricular preexcitation, the Wolff-Parkinson-White syn- drome. AF with bundle branch block is the likely diagnosis when the ventricular rate is approximately 120-160 bpm and the QRS morphol- ogy is consistent with RBBB or LBBB (Fig. 1). AF with ventricular preexcitation should be considered when the ventricular rate is exces- sive (e.g., >=180 bpm) and the QRS morphology is bizarre (Figs. 1 and 5). This scenario is frequently called “FBI” for fast, broad-complex and ir- regular [30]. However, AF with bundle branch block is also fast, broad- complex and irregular. The abbreviation FBI can be kept but it should stand for fast, bizarre and irregular. The term “pseudoventricular tachy- cardia” is also appropriate because the QRS morphology usually looks like VT but the irregular rhythm suggests that it is not VT (Fig. 5). In ir- regular WCT, fusion complexes reflect ventricular activation through the AV node and, simultaneously, through an Accessory pathway and therefore are diagnostic of AF with WPW (Fig. 5).
With irregular WCTs too, the clinical presentation is important. AF with bundle branch block is more likely in elderly patients and in pa- tients with structural heart disease. AF with ventricular preexcitation is more common in patients without structural heart disease (Fig. 5). With irregular WCT, however, the Clinical context is less predictive of the cause of the tachycardia than in regular WCT. Hence, the ECG char- acteristics are more important in distinguishing AF with bundle branch block vs. AF with ventricular preexcitation (Fig. 1).
Sustained irregular ventricular tachycardia is rare. Ventricular tachy- cardia as the cause of an irregular WCT should be suspected in elderly patients with structural heart disease when the QRS morphology is bi- zarre but the ventricular rate is relatively slow such as 120 bpm. In such cases, as in regular WCT, it is useful to search for signs of AV disso- ciation which would nail down the diagnosis of VT.
Therapy
AF with bundle branch block should be treated according to atrial fi- brillation guidelines. The initial step should be ventricular Rate control with IV diltiazem or beta blocker (Fig. 1) [20]. If AF with WPW is suspected, the most important decision is to avoid AV nodal blocking agents such as IV adenosine, verapamil, diltiazem, Beta blockers and di- goxin (Fig. 1). The use of IV amiodarone can also be detrimental [31]. As is the case with regular WCT, here too electric cardioversion is a reason- able initial treatment option, especially if the heart rate is very fast or the patient has poor left ventricular systolic function (Fig. 1). After seda- tion with etomidate or propofol, monophasic shock should be delivered at 200 joules and biphasic shock at 120-200 joules [20]. If pharmaco- logic therapy is chosen, the first line agent should be IV procainamide which can suppress conduction through the accessory pathway (Fig. 1). IV ibutilide or, in very stable patients, oral flecainide or propafenon can also be used.
Applicability and limitations
This review is only applicable to the adult patient who presents with clinically stable monomorphic WCT. It was not our purpose to elaborate on the evaluation and management of polymorphic VT, pulseless WCT or Electrical storm. Our approach is primarily intended for care

Fig. 5. ECG recorded from a 44-year-old woman with no known heart disease who presented with palpitation and lightheadedness. Note the irregularly irregular ventricular rhythm at a rate of 178 bpm, the bizarre QRS morphology resembling VT (deep negative QRS complexes in lead I; QRS concordance in the chest leads), and the occasional presence of narrower QRS complexes consistent with fusion beats (F). This clinical and ECG scenario was typical for atrial fibrillation and ventricular preexcitation, the Wolff-Parkinson-White syndrome.
delivered in the emergency department by emergency medicine practi- tioners (EMPs). This approach may be preferable in this setting to ACLS guidelines given that (1) acute management of arrhythmias should be an area of relative expertise for EMPs and (2) by definition, stable ar- rhythmia will allow for the minimal time required to collect such his- tory as demographics and prior cardiovascular conditions. It is uncertain if our recommendations lend themselves to settings other than the emergency department as, for instance, in an intensive care unit where the proportions outlined here for regular WCT (i.e., 80% of regular WCT is VT) may not apply.
The presented approach does not cover rare forms of WCT such as WPW with antidromic reentrant supraventricular tachycardia or regu- lar pre-excited atrial tachycardia [32-34]. These diagnoses, however, are almost never made at the initial clinical encounter. In addition, such conditions typically present with regular WCT resembling VT, and the use of IV procainamide is appropriate.
Our approach to the initial evaluation and management of stable WCT has not been systematically tested for accuracy and patient out- comes. It would be useful to perform a prospective study in the real- life setting to test what proportion of WCT ECGs will still be ambiguous after evaluation as illustrated in Fig. 1, and to track the outcomes of pa- tients who were managed according to the described approach.
Summary
In cases of WCT, the ECG should never be evaluated without consid- eration of the clinical context. Regular WCT in elderly patients and in pa- tients with structural heart disease is almost always VT. Demonstration of an inconsistent P-QRS relationship essentially confirms the diagnosis of VT. If the rate is very fast or the patient has poor left ventricular sys- tolic function, electric cardioversion should probably be performed. If the rate is not excessive and the tachycardia is tolerated, give IV pro- cainamide. In younger patients with no known heart disease, especially if the QRS morphology resembles bundle branch block, SVT is somewhat more likely; prove it with IV adenosine. Irregular WCT in an elderly pa- tient and in the patient with structural heart disease is almost always AF with bundle branch block; treat it according to AF guidelines. In patients with no known heart disease, especially when the ventricular rate is very fast and the QRS complexes are bizarre (fast, bizarre, irregular -
FBI), AF with WPW is the likely diagnosis. When the heart rate is exces- sive or the patient has poor left ventricular systolic function, direct cur- rent electric cardioversion should be employed. If the ventricular rate is not excessive and the tachycardia is tolerated, treat it with IV procain- amide. Patients with any type of WCT that causes clinical or hemody- namic instability should undergo immediate electric cardioversion.
References
- Alzand BSN, Crijns HJGM. Diagnostic criteria of broad complex tachycardia: decades of evolution. Europace 2011;13:465-72.
- Brady WJ, Mattu A, Tabas J, Ferguson JD. The differential diagnosis of wide QRS com- plex tachycardia. Am J Emerg Med 2017;35:1525-9.
- Hollowell H, Mattu A, Perron AD, Holstege C, Brady WJ. Wide-complex tachycardia: beyond the traditional differential diagnosis of ventricular tachycardia vs supraven- tricular tachycardia with aberrant conduction. Am J Emerg Med 2005;23:876-89.
- Dancy M, Camm AJ, Ward D. Misdiagnosis of chronic recurrent ventricular tachycar- dia. Lancet 1985;326:320-3.
- Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and out- come after emergent therapy. Ann Intern Med 1986;104:766-71.
- Baerman JM, Morady F, DiCarlo Jr LA, de Buitler M. Differentiation of ventricular tachycardia from supraventricular tachycardia with aberration: value of the clinical history. Ann Emerg Med 1987;16:40-3.
- Steinman RT, Herrera C, Schuger CD, Lehmann MH. Wide QRS tachycardia in the conscious adult: ventricular tachycardia is the most frequent cause. JAMA 1989; 261:1013-6.
- Reinelt P, Karth G, Geppert A, Heinz G. Incidence and type of cardiac arrhythmias in critically ill patients: a single center experience in a medical-cardiological ICU. Inten- sive Care Med 2001;27:1466-73.
- Goldberger ZD, Rho RW, Page RL. Approach to the diagnosis and initial management of the stable adult patient with a wide complex tachycardia. Am J Cardiol 2008;101: 1456-66.
- Garner JB, Miller JM. Wide complex tachycardia - ventricular tachycardia or not ven- tricular tachycardia, that remains the question. Arrhythmia Electrophysiol Rev 2013; 2:23-9.
- Tchou P, Young P, Mahmud R, Denker S, Jazayeri M, Akhtar M. Useful clinical criteria for the diagnosis of ventricular tachycardia. Am J Med 1988;84:53-6.
- Akhtar M, Shenasa M, Jazayeri M, Caceres J, Tchou PJ. wide QRS complex tachycar- dia: reappraisal of a common clinical problem. Ann Intern Med 1988;109:905-12.
- Vereckei A. Current algorithms for the diagnosis of Wide QRS complex tachycardias. Curr Cardiol Rev 2014;10:262-76.
- Jastrzebski M, Kukla P, Czarnecka D. Ventricular tachycardia score: a novel method for wide QRS complex tachycardia differentiation - explained. J Electrocardiol 2017;50:704-9.
- El Hajjai I, Becker G, Kus T, Vinet A, Berkovitz A, Sturmer M. Novel criterion for the differential diagnosis of wide QRS complexes and wide complex tachycardia using the initial activation of QRS on leads V1 and V2: differential diagnosis of wide QRS based on V1-V2. J Electrocardiol 2018;51:700-6.
- Isenhour JL, Craig S, Gibbs M, Littmann L, Rose G, Risch R. Wide-complex tachycar- dia: continued evaluation of diagnostic criteria. Acad Emerg Med 2000;7:769-73.
- Jastrzebski M, Kukla P, Czarnecka D, et al. Comparison of five electrocardiographic methods for differentiation of wide QRS-complex tachycardias. Europace 2012;14: 1165-71.
- Baxi RP, Hart KW, Vereckei A, Miller J, Chung S, Chang W, et al. Vereckei criteria as a diagnostic tool amongst emergency medicine residents to distinguish between ven- tricular tachycardia and supra-ventricular tachycardia with aberrancy. J Cardiol 2012;59:307-12.
- May AM, Brenes-Salazar JA, DeSimone CV, Vaidya VR, Ternus BW, Hodge DO, et al. Electrocardiogram algorithms used to differentiate wide complex tachycardias dem- onstrate diagnostic limitations when applied by non-cardiologists. J Electrocardiol 2018;51:1103-9.
- Morrison LJ, Deakin CD, Morley PT, Callaway CW, Kerber RE, Kronick SL, et al. Part 8: advanced life support: 2010. International consensus on cardiopulmonary resuscita- tion and Emergency Cardiovascular Care Science with treatment recommendations. Circulation 2010;122:S345-421.
- Lau EW, Pathamanthan RK, Ng GA, Cooper J, Skehan JD, Griffith MJ. The Bayesian ap- proach improves the electrocardiographic diagnosis of broad complex tachycardia. Pacing Clin Electrophysiol 2000:1519-26.
- Zauner CA, Holshouser JW, Littmann L. Ventricular tachycardia and electrocardio- graphic ST-segment-elevation myocardial infarction without coronary artery dis- ease. Circulation 2018;137:1287-9.
- Brady WJ, Skiles J. Wide QRS complex tachycardia: ECG differential diagnosis. Am J Emerg Med 1999;17:376-81.
- Griffith MJ, Ward DE, Linker NJ, Camm AJ. Adenosine in the diagnosis of broad com- plex tachycardia. Lancet 1988;331:672-5.
- Ortiz M, Martin A, Arribas F, Coll-Vinent B, Del Arco C, Peinado R, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J 2017;38:1329-35.
- Marill KA, Wolfram S, deSouza IS, Nishijima DK, Kay D, Setnik GS, et al. Adenosine for wide-complex tachycardia: efficacy and safety. Crit Care Med 2009;37:2512-8.
- Trohman RG, Parrillo JE. Direct current cardioversion: indications, techniques, and
recent advances. Crit Care Med 2000;28(10 Suppl):N170-3.
Choi GJ, Kang H, Baek CW, Jung YH, Ko JS. Etomidate versus propofol sedation for electric cardioversion: a meta-analysis. Curr Med Res Opin 2018;34:2023-9.
- deSouza IS, Martindale JL, Sinert R. Antidysrhythmic drug therapy for the termina- tion of stable, monomorphic ventricular tachycardia: a systematic review. Emerg Med J 2015;32:161-7.
- Richter S, Brugada P. FBI (fast broad irregular): a case for the secret service? Circu- lation 2006;114:e638-9.
- Nebojsa M, Dragan S, Nebojsa A, Tamara A. lethal outcome after intravenous admin- istration of amiodarone in patient with atrial fibrillation and ventricular preexcitation. J Cardiovasc Electrophysiol 2011;22:1077-8.
- Megid TBC, Palmegiani E, Lorga-Filho AM. Wide QRS complex tachycardia in patients with Chagas’ disease: sustained ventricular tachycardia until proven otherwise. J Electrocardiol 2018;51:756-9.
- Nair KKM, Namboodiri N, Abhilash SP, Valaparambil. RBBB tachycardia with north- west axis: what is the mechanism? J Electrocardiol 2018;51:121-5.
- Topaloglu S, Ozeke O, Cay S, Ozcan F, Koca S, Aras D. Wide QRS complex supraven- tricular tachycardia with negative precordial concordance: electrocardiographic clues for Mahaim pathway with Ebstein anomaly. J Electrocardiol 2018;51:663-6.
