Comparison of supine and upright face-to-face cadaver intubation
a b s t r a c t
Introduction: Optimal patient positioning during intubation improves laryngeal view and First pass success, as well as reducing incidence of hypoxia. In certain pre-hospital situations, it may be impractical or impossible for the operator to stand behind the patient.
Objective: We compared intubation in the supine and upright face-to-face positions, with regards to time to in- tubate and the view of the vocal cords obtained.
Methods: This was a pilot comparison study. One investigator intubated 25 cadavers with the use of a bougie in the supine and upright face-to-face positions. Each attempt was recorded on a video laryngoscope. Recordings of each attempt were reviewed by five blinded emergency physicians, who allocated both a percentage of Glottic opening (POGO) score and Cormack-Lehane (CL) grade. Time to insertion of the endotracheal tube through the vocal cords was measured from the video.
Results: The median intubation time was 1 s longer for upright cadavers than for supine cadavers, with greater variation in intubation times for upright cadavers compared with supine cadavers (IQR 9.0 vs 3.5 excluding the outlier case). The mean POGO score (averaged across raters) was 4.7% lower for upright intubation attempts (excluding the outlier case) with a moderate-to-good degree of inter-rater reliability, however this difference was not statistically significant. The median CL grade (averaged across raters) was 0.2 higher for upright intuba- tion attempts (excluding the outlier case) with a poor-to-moderate degree of inter-rater reliability, and this dif- ference was also not statistically significant.
Conclusions: This pilot study suggests that upright, face-to-face intubation may be clinically similar to supine in-
tubation in terms of time to intubation and difficulty. Further studies utilising a larger number of operators and cadaver types are indicated.
(C) 2022
Patients who require emergent endotracheal intubation in the emer- gency department (ED) are commonly positioned supine, with recent data from the Australia and New Zealand ED Airway Registry suggesting 72% of ED patients are intubated either flat or with an occipital pad or pillow only. Notably, only 13% of patients in this study were ramped [1]. The ramped position has been found to improve laryngeal view when compared to a standard “sniff” position in the morbidly obese
E-mail address: [email protected] (D. Julliard).
population [2]. It has been shown that patients who are pre-oxygenated in the head-up or sitting positions are more tolerant to apnea when compared with the supine position [3-6]. Importantly, these findings are relevant to the obese and severely obese patient populations [3,4], for whom hypoxia is a more common complication of intubation [7]. This is due to increasing the patient’s functional residual capacity by shifting the abdominal contents away from the diaphragm and reducing the effect of the gravity on the chest wall [2,7].
When patients are positioned in the ramped or sitting positions, the laryngoscopist may be required to stand up on a stool behind the patient and lean forwards over the head to obtain a view of the larynx – stand- ing next to the patient may be felt to be ergonomically easier [new ref- erence]. Furthermore, a small subset of patients in the pre-hospital
https://doi.org/10.1016/j.ajem.2022.03.029
0735-6757/(C) 2022
environment may benefit from intubation whilst upright, for example a prolonged extrication of a patient from a car who is trapped in a seat and has respiratory failure, or patients who are trapped in such a position that the intubating clinician cannot position themselves behind the pa- tients head as may happen in some industrial accidents with trapped patients.
The C-Mac (Karl Storz, GmbH & Co. KG, Tuttlingen, Germany), like other video laryngoscopes with a screen separate from the blade, allows the laryngoscopist to stand away from their traditional position behind the patient’s head. We postulate that it is possible, when using a video laryngoscope such as the C-Mac, to intubate an upright patient whilst standing in front of them.
In assessing the feasibility of upright face-to-face intubation, many studies have employed simulation manikins [8-11]. These studies have shown improvement in time for and success of first-pass intubation in upright positions when compared to the supine positioning [8,11]. Clearly, these studies are limited in that all procedures are performed on manikins, and hence lose the ability to truly assess the effect of posi- tion change on human tissue.
With growing evidence for advantages of upright positioning, it is im- portant to evaluate whether position modification for intubation causes any significant change to the time taken for and success of intubation. This study aimed to compare the efficacy of intubation of cadavers in the upright face-to-face position compared with the traditional supine position.
- Methods
- Study design
This was a comparison study that was approved by Northern Sydney Local Health District Human Research Ethics Committee in March 2014 (LNR/13/HAWKE/435).
A single investigator (TF) intubated 25 cadavers in both the supine and in the upright face-to-face position in a random order with the use of a bougie. The decision to proceed with a single intubator was in- fluenced by the fact that the cadaver tissue tended to start to mould to the shape of the laryngoscopy blade. Increasing the number of operators for this pilot study would reduce the generalisability of this study due to the manipulation of the cadaver tissue. TF is a senior emergency physi- cian (EP) and prehospital and retrieval specialist. Between these two roles, TF intubates patients approximately 20 times per year, which is consistent with, or above, the average for EPs in Australia [1]. Of note, TF was very familiar with the practice of video laryngoscopy, using it ex- clusively in their clinical practice.
Each attempt was recorded on a C-Mac video laryngoscope. Re- cordings of the intubation attempts were timed from the moment the Laryngoscope blade first entered the mouth to the time the tip of the Endotracheal tube was seen to pass through the vocal cords. As is standard practice in many protocols for emergency intu- bation, including all those at our institution [12], a bougie was used for all attempts.
The cadavers were purchased by the Sydney Clinical Skills and Sim- ulation Centre for an Emergency Airway Workshop. They were a mix- ture of male/female from different ethnic backgrounds. The cadavers had been frozen (and not preserved in formaldehyde), which en- sured that their tissues were as near as to the condition of body tis- sue in life. Each cadaver comprised of head and torso, which was placed on a purpose-built stand that could be positioned flat or up- right to 60 degrees. A small pad was placed behind each cadaver’s occiput in order to maintain the cervical spine in the neutral posi- tion in all cases. The stand was placed on a trolley and the laryngoscopist stood behind the cadaver for supine positioning (see Fig. 1), whilst for the upright position, the laryngoscopist stood to the right-hand side of the cadaver and leant across to gain an almost “face-to-face” position (see Fig. 2). Importantly, the
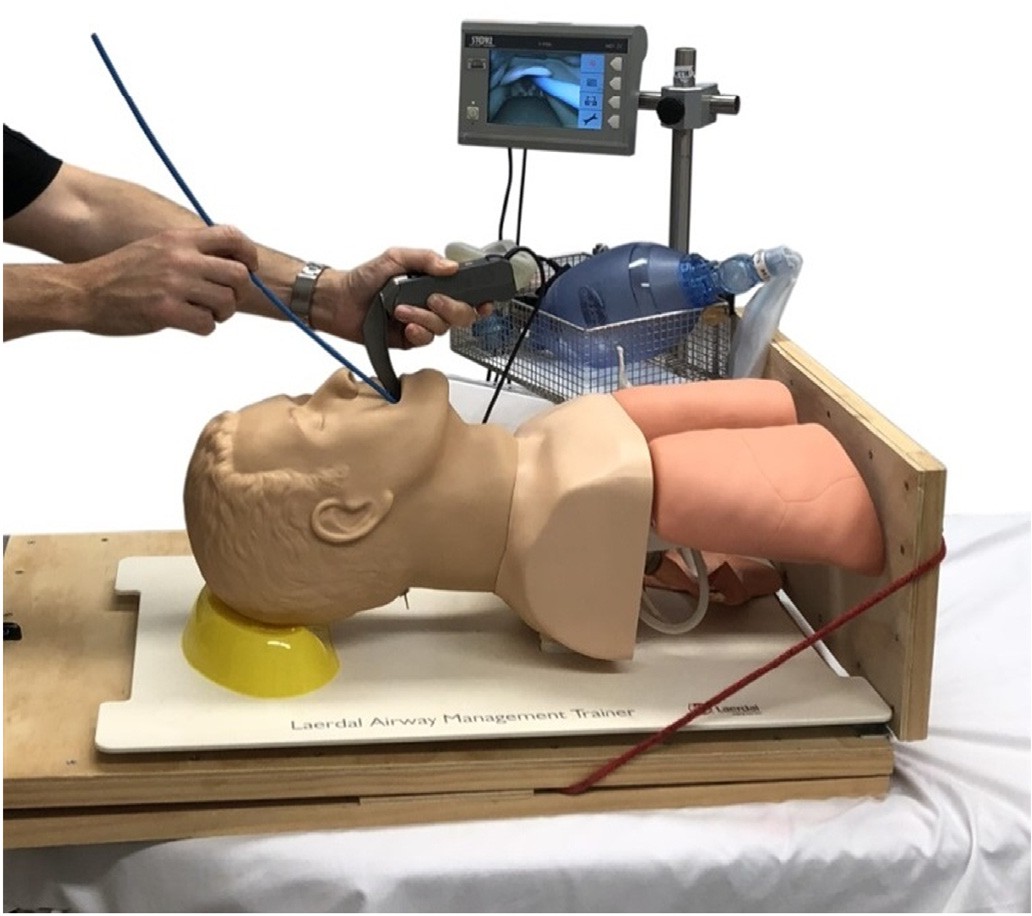
Fig. 1. Supine positioning.
flanged design of the C-Mac blade, which is in keeping with tradi- tional Macintosh blades, allows the patient’s tongue to be swept to the left. When in the face-to-face position, this design feature re- quires the laryngoscope to be held in the right hand in order to sweep the patient’s tongue to the left.
The recordings of each intubation attempt were reviewed by five EPs who were blinded to the position of the cadaver. The position of the ca- daver was concealed on the video as recording was only commenced when the laryngoscope was positioned immediately in front to the mouth, so there was nothing in the background of the video that would give clues as to the position of the cadaver. Each EP allocated both a percentage of glottic opening (POGO) score [13] and Cormack- Lehane (CL) grade [14], using a standardized aide to ensure consistency of grading.
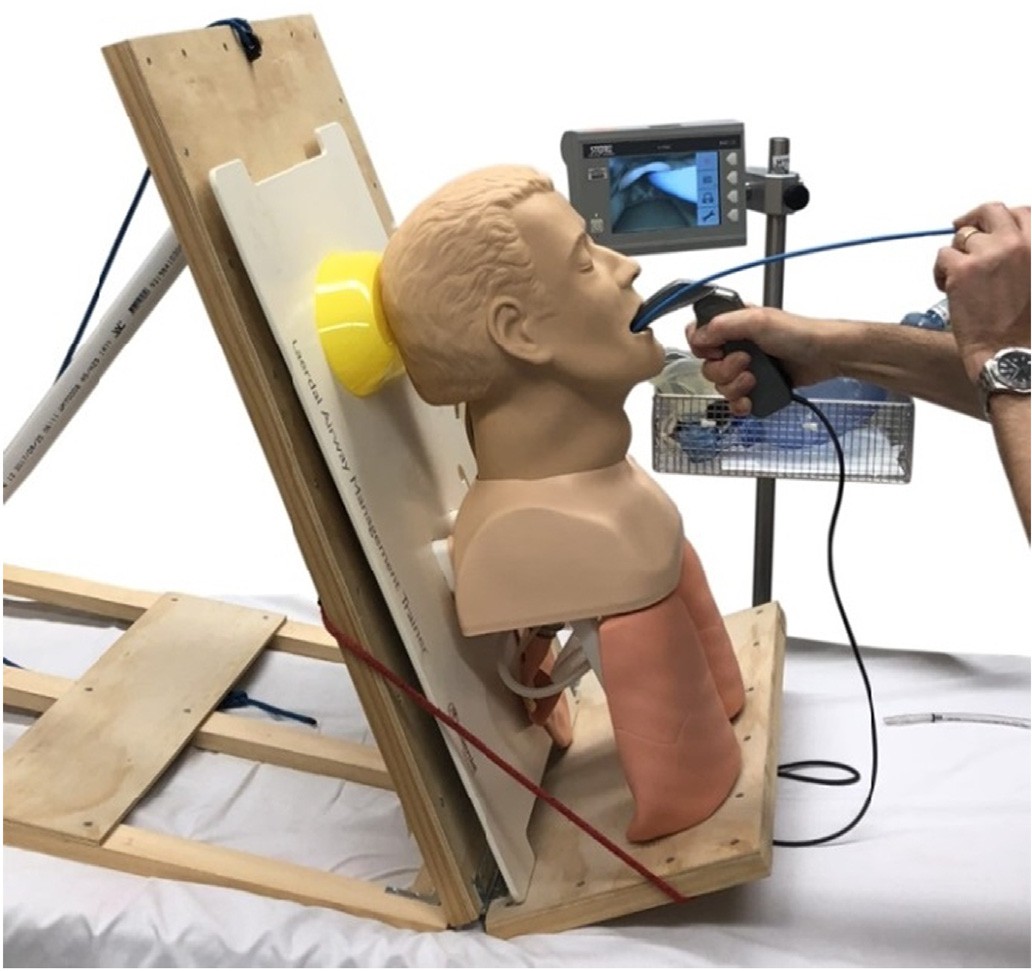
Fig. 2. Upright face-to-face positioning.
The primary outcome was time to intubation, which was calculated from the time the laryngoscope blade entered the mouth at the first at- tempt to the time the ETT was passed through the vocal cords.
The secondary outcome was a comparison of the laryngeal views ob- tained in the supine and upright positions using both POGO score and CL grade. The POGO score is a continuous measure ranging from 0% to 100%, with higher values indicating a greater degree of intubation suc- cess. On the other hand, the CL grade is an ordinal measure that is re- ported on a scale ranging from 1 to 4, with lower values indicating a greater degree intubation success (noting that no cases in this study were scored with a CL grade of 4, which would have indicated that nei- ther the glottis nor epiglottis were visible).
-
- Data analysis
Data processing and analysis were performed using R statistical soft- ware (v3.4).
When analysing the POGO score and CL grade outcomes, the average of the five rater assessments for each cadaver-position case were first computed, with descriptive analysis and statistical inference then per- formed on the average scores.
To assess the inter-rater reliability amongst the five evaluators, the single-rating absolute-agreement intraclass correlation coefficient was calculated using a two-way random effects model, with the specification following the guidelines outlined in Koo and Li [18] and Trevethan [19] and statistics estimated using the IRR package v0.84.1 in R. In particular, the ICC was chosen as the inter-rater reliability mea- sure of interest as it can be applied to analyse situations where there are more than two raters.
Given the relatively small sample size, quantile-quantile (QQ) plots and the Shapiro-Wilk test were used to analyse the distributions of the continuous measures of interest to identify deviations from normal- ity. Where variables were measured on an ordinal scale or found to be non-normal, the median and interquartile range (IQR) were reported and a paired Wilcoxon signed-rank test (pairing between supine and upright positions) used to analyse differences in outcomes. Where var- iables were not found to deviate significantly from a normal distribu- tion, the mean and standard deviation (SD) were reported and a paired t-test (pairing between supine and upright positions) applied to analyse differences in outcomes. Analysis was performed both in- cluding and excluding measurements on a cadaver where there was an outlier value for the upright intubation time. In each case, test out- comes were reported as 95% confidence intervals (CI).
- Results
- Descriptive statistics
While the study design initially included 50 intubation attempts, there were 48 video recordings ultimately included in the study (24 su- pine and 24 upright) due to a failure in the video recording for a single upright intubation attempt, with the corresponding supine intubation attempt on the same cadaver also excluded from the analysis. Table 1 presents the findings of this study, both including and excluding the outlier case.
Further, a single cadaver required two intubation attempts in the up- right position, which resulted in an outlier intubation time value of 124 s. We have therefore analysed the data both including and exclud- ing the upright and supine intubation attempts on this cadaver.
-
- Analysis of intubation time
Visual inspection of QQ plots suggested that the distribution of intu- bation times was right-skewed, with the Shapiro-Wilk test indicating a deviation from normality (Supine: W = 0.73, p < 0.01; Upright: W = 0.53, p < 0.01). Therefore, the median and IQR were used to summarise this variable, with the paired Wilcoxon signed-rank test (pairing be- tween supine and upright positions for each cadaver) applied to test for differences in intubation times. The median intubation time (both including and excluding the outlier) was 1 s longer for the upright vs. supine populations, with a greater variation in intubation times for up- right cases compared with supine cases (Including outlier: IQR 9.8 vs. 3.4, Excluding outlier: IQR 9.0 vs 3.5). Applying the Wilcoxon signed- rank test, we found evidence that the difference between upright and supine intubation times was statistically significant (95% CI including outlier: 2.0-12.5, 95% CI excluding outlier: 1.5-9.5). However, this dif- ference is unlikely to have significant clinical implications.
-
- Analysis of views obtained
For each of the 48 intubation attempts (46 excluding the cadaver with the outlier intubation time in the upright position), 5 rater assess- ments were obtained for the POGO score as well as the CL grade.
For each score, the single-rating absolute-agreement ICC was calcu- lated using a two-way random effects model to assess the inter-rater re- liability, which indicated a poor-to-moderate degree of inter-rater reliability when assessing CL grades (95% CI including and excluding in- tubation time outlier: 0.33-0.66) and a moderate-to-good degree of inter-rater reliability when assessing POGO scores (95% CI including
Descriptive statistics
Measure Descriptive statistics
Median (IQR) reported for Intubation time and Averaged CL grade, Mean (SD) reported for Averaged POGO score
Supine Upright
95% CI for Upright – Supine Inter-rater reliability: 95% CI for ICC
|
Including cadaver with outlier case (n = 48; Supine = 24, Upright = 24) |
||||
|
Intubation time |
19.0 |
20.0 |
2.0-12.5 |
N/A |
|
Averaged CL grade |
(17.8-21.3) 1.6 |
(18.0-27.8) 1.8 |
-0.4-0.1 |
0.33-0.66 |
|
Averaged POGO score |
(1.2-2.0) 61.8 |
(1.4-2.1) 55.1 |
-6.2-19.7 |
0.64-0.84 |
|
(26.4) |
(30.2) |
|||
|
Excluding cadaver with outlier case (n = 46; Supine = 23, Upright = 23) |
||||
|
Intubation time |
19.0 |
20 |
1.5-9.5 |
N/A |
|
Averaged CL grade |
(17.5-21.0) 1.6 |
(18.0-27.0) 1.8 |
-0.4-0.2 |
0.33-0.66 |
|
Averaged POGO score |
(1.2-2.0) 61.7 |
(1.3-2.0) 57.0 |
-8.1-17.5 |
0.64-0.85 |
|
(27.0) |
(29.3) |
|||
intubation time outlier: 0.64-0.84, 95% CI excluding intubation time outlier: 0.64-0.85).
CL grades were summarised using the median and IQR given the or- dinal scale of the variable, with the paired Wilcoxon signed-rank test (pairing between supine and upright positions for each cadaver) used to test for differences in the averaged CL grades. The median of the av- eraged CL grade was 0.2 higher for the upright vs. supine populations (both including and excluding the intubation time outlier), with a slightly greater variation in CL grades for upright cases compared with supine cases (Including and excluding outlier: IQR 0.8 vs 0.7). Applying the Wilcoxon signed-rank test, we did not find evidence that the differ- ence between upright and supine averaged CL grades was statistically significant (95% CI including intubation time outlier: -0.4-0.1, 95% CI excluding intubation time outlier: -0.4-0.2).
An inspection of QQ plots and application of the Shapiro-Wilk test did not find evidence that the POGO score distributions deviated signif- icantly from normality (Supine: W = 0.93, p = 0.08, Upright: W = 0.94, p = 0.15), and this variable was therefore summarised using the mean and standard deviation with the paired t-test (pairing between supine and upright positions for each cadaver) used to test for differences in av- eraged POGO scores. The mean of the averaged POGO score was 6.7% lower for the upright vs. supine populations when including the cadaver with the intubation time outlier, and 4.7% lower when excluding this cadaver. Applying the paired t-test, we did not find evidence that this difference was statistically significant (95% CI including outlier:
-6.2-19.7, 95% CI excluding outlier: -8.1-17.5).
- Discussion
Recent studies have contested the previously unchallenged suitabil- ity of supine positioning for emergency intubations. Turner et al. dem- onstrated a higher rate of success in the upright position amongst residents performing intubations in the emergency department. Emer- gency medicine residents intubating patients with the head of the bed el- evated to 45? or higher had a high rate of first pass success and high rates of satisfaction with patient positioning [15]. In emergent situations, Khandelwal et al. found that intubating with the head of the bed elevated above 30? was associated with decreased peri-intubation complications, in particular decreased rates of hypoxemia and aspiration [16].
These two studies recognized the limitations of their study designs in accounting for the possibility that patients intubated in the supine position were more unstable, particularly when active cardiopulmonary resuscitation was underway.
The majority of other existing studies examining feasibility of non- supine positioning have been performed in context of elective surgical patients undergoing endotracheal intubation in controlled circum- stances [3-6]. Lee et al. demonstrated improvement in laryngeal view through achievement of increased POGO scores in the 25? back-up posi- tion compared with flat supine position in a study on elective surgical patients [17].
This study aimed to add to the current body of evidence by compar- ing times and views obtained during supine and upright face-to-face in- tubation conducted on human tissue without the influence of confounding clinical factors (e.g. active cardiopulmonary resuscitation). Intubation time was found to be marginally longer for upright ca- davers, however, the median difference of 1 s is unlikely to have signif- icant clinical implications. There was a single outlier case that required two attempts to intubate in the upright position and took significantly longer than the remaining attempts in either position, with the diffi- culty encountered being attributed to challenges in manipulating the bougie. This was likely due to the relative unfamiliarity with intubation in the upright, face-to-face position and the need to hold the laryngo- scope in the right hand. We hypothesize that this unfamiliarity with the technique also accounts for the greater variation in intubation times for upright cadavers compared to supine (Including outlier: IQR 9.8 vs. 3.4, Excluding outlier: IQR 9.0 vs 3.5). Comparing the intubation
outcomes between supine vs. upright populations, we found marginal differences in the median averaged CL grades (0.2 higher for upright) and median averaged POGO scores (6.7% lower for upright), however these differences were not statistically significant and are unlikely to represent substantial clinical differences in the intubation success rate. The feasibility of upright face-to-face intubation is important for as- sessment due to two important emergency applications. Firstly, in the pre-hospital setting where airway management can provide unique challenges of limited access and mobility, necessitating modification of approach and use of upright techniques. Exploration of this approach provides an option for situations where position is likely to be subopti- mal. Secondly, for patients with Disease states that predispose them to Oxygen desaturation in the supine position, whom require emergent
intubation.
Combined with recent literature indicating upright positioning is as- sociated with reduced risk of intubation-related complications, the find- ings of this study indicate that more consideration should be given to the upright position for intubation in emergent situations. Whilst the findings do not support routinely altering position for intubation, they do provide reassurance if upright positioning is chosen for optimization for other reasons. The importance of the practitioner having a high de- gree of familiarity with a technique has a huge impact on a high- stakes procedure such as endotracheal intubation. Demonstrating parity in the practical components of time and views obtained provides an ar- gument for more formal training in airway management in the upright position.
-
- Limitations
This comparison study was conducted with the use of a single laryngoscopist as a pilot investigation into the feasibility of upright face-to-face intubation. We recognize that this has limited the general- izability of the results and calls for further studies utilising a larger num- ber of operators and cadaver types are indicated.
- Conclusions
From the findings of this study, we demonstrated minimal difference in the time to intubation or difficulty according to intubation grade in the upright face-to-face position when compared to the supine position. These differences are unlikely to be clinically significant. Upright posi- tioning has been found to have clinical benefits for certain patient pop- ulations, and needs further study for application in emergent situations.
Funding
This research did not receive any specific grant from funding agen- cies in the public, commercial, or not-for-profit sectors.
Declarations of interest
None.
Acknowledgements
We would like to acknowledge the efforts of our blinded reviewers: Dr. Rachel Vassiliadis, Dr. Tom Harwood, Dr. Joanne Oo and Dr. Rachel Michie. We are also grateful to the staff of the Sydney Clinical Skills Cen- tre for their assistance with this project.
References
- Alkhouri H, et al. Emergency airway management in Australian and New Zealand emergency departments: a multicentre descriptive study of 3710 emergency intu- bations. Emerg Med Aust. 2017;29(5):499-508.
- Collins JS, et al. Laryngoscopy and morbid obesity: a comparison of the “sniff” and
“ramped” positions. Obes Surg. 2004;14(9):1171-5.
- Altermatt FR, et al. Pre-oxygenation in the obese patient: effects of position on toler- ance to apnea. Br J Anaesth. 2005;95(5):706-9.
- Dixon BJ, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;102(6):1110-5. [discussion 5A].
- Lane S, et al. A prospective, randomised controlled trial comparing the efficacy of pre-oxygenation in the 20 degrees head-up vs supine position. Anaesthesia. 2005; 60(11):1064-7.
- Ramkumar V, Umesh G, Philip FA. Preoxygenation with 20 masculine head-up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese Healthy adults. J Anesth. 2011;25(2):189-94.
- Murphy C, Wong DT. Airway management and oxygenation in obese patients. Can J Anaesth. 2013;60(9):929-45.
- Amathieu R, et al. Simulating face-to-face tracheal intubation of a trapped patient: a randomized comparison of the LMA Fastrach™, the GlideScope™, and the Airtraq™ laryngoscope. Br J Anaesth. 2012;108(1):140-5.
- Gaszynska E, et al. Intubation by paramedics using the ILMA or AirTraq, KingVision, and Macintosh laryngoscopes in vehicle-entrapped patients: a manikin study. Eur J Emerg Med. 2014;21(1):61-4.
- Grosomanidis V, et al. Comparison between intubation through ILMA and Airtraq, in different non-conventional patient positions: a manikin study. Emerg Med J. 2012; 29(1):32-6.
- Venezia D, et al. Comparison of sitting face-to-face intubation (two-person tech- nique) with standard oral-tracheal intubation in novices: a Mannequin study. J Emerg Med. 2012;43(6):1188-95.
- Fogg T, Alkhouri H, Vassiliadis J. The Royal North Shore Hospital Emergency Depart- ment airway registry: closing the audit loop. Emerg Med Australas. 2016;28(1): 27-33.
- Levitan RM, et al. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med. 1998;5(9):919-23.
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39(11):1105-11.
- Turner JS, et al. Feasibility of upright patient positioning and intubation success rates at two academic EDs. Am J Emerg Med. 2017;35(7):986-92.
- Khandelwal N, et al. Head-elevated patient positioning decreases complications of emergent tracheal intubation in the ward and intensive care unit. Anesth Analg. 2016;122(4):1101-7.
- Lee BJ, Kang JM, Kim DO. Laryngeal exposure during laryngoscopy is better in the 25 degrees back-up position than in the supine position. Br J Anaesth. 2007;99(4): 581-6.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coeffi- cients for reliability research. J Chiropr Med. 2016 Jun;15(2):155-63.
- Trevethan R. Intraclass Correlation coefficients: clearing the air, extending some cau- tions, and making some requests. Health Serv Outcomes Res Methodol. 2017;17: 127-43.
